What's so great about fruits and vegetables?
For generations, we have known that fruits and vegetables are good for our health. Multiple studies show time and again that we live longer when we eat more…

Update your location to show providers, locations, and services closest to you.
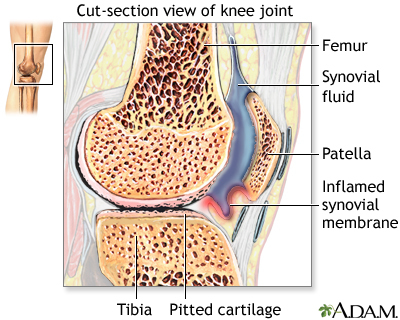
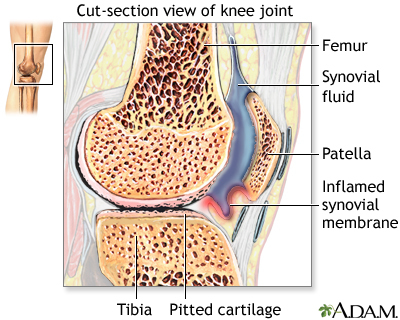
Rheumatoid arthritis (RA) is a disease that leads to inflammation of the joints and surrounding tissues. It is a long-term disease. It can also affect other organs.
RA; Arthritis - rheumatoid
The cause of RA is not known. It is an autoimmune disease. This means the immune system of the body mistakenly attacks healthy tissue.
RA can occur at any age, but is more common in middle age. Women get RA more often than men.
Infection, genes, and hormone changes may be linked to the disease. Smoking may also be linked to RA.
It is less common than osteoarthritis (OA). OA which is a condition that occurs in many people due to wear and tear on the joints as they age.
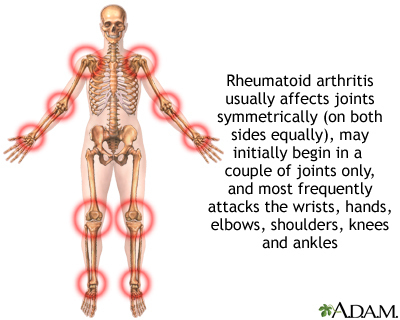
Most of the time, RA affects joints on both sides of the body equally. Fingers, wrists, knees, feet, elbows, ankles, hips and shoulders are the most commonly affected.
The disease often begins slowly. Early symptoms may include:
Joint symptoms may include:
Other symptoms include:
The diagnosis of RA is made when:
Sometimes the diagnosis of RA is made even without all of the conditions shown above if the arthritis is otherwise typical for RA.
There is no test that can determine for sure whether you have RA. Most people with RA will have some abnormal test results. However, some people will have normal results for all tests.
Two lab tests that are positive in most people and often help in the diagnosis are:
These tests are positive in most patients with RA. The anti-CCP antibody test is more specific for RA.
Other tests that may be done include:
RA most often requires long-term treatment by an expert in arthritis called a rheumatologist. Treatment includes:
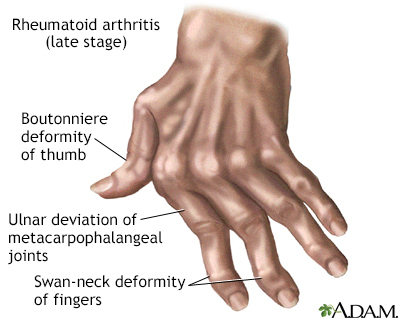
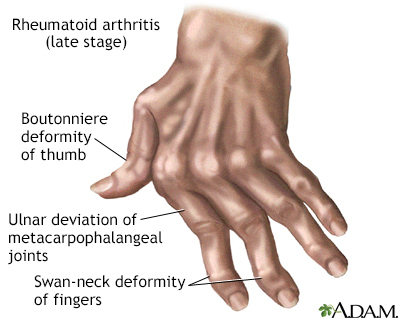
Early treatment for RA with medicines called disease-modifying antirheumatic drugs (DMARDS) should be used in all patients. This will slow joint destruction and prevent deformities. The activity of the RA should be checked at regular visits to make sure the disease is under control. The goal of treatment is to stop the progression of the RA.
MEDICINES
Anti-inflammatory medicines: These include aspirin and nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, naproxen and celecoxib.
Disease modifying antirheumatic drugs (DMARDs): These are often the medicines that are tried first in people with RA. They are prescribed along with rest, strengthening exercise, and anti-inflammatory drugs.
Corticosteroids -- These medicines work very well to reduce joint swelling and inflammation, but they can have long-term side effects. Therefore, they should be taken only for a short time and in low doses when possible.
Biologic DMARD agents -- These medicines are designed to affect parts of the immune system that play a role in the disease process of RA.
Biologic and synthetic agents can be very helpful in treating RA. However, people taking these medicines must be watched closely because of uncommon, but serious adverse reactions:
SURGERY
Surgery may be needed to correct severely damaged joints. Surgery may include:
PHYSICAL THERAPY
Range-of-motion exercises and exercise programs prescribed by a physical therapist can delay the loss of joint function and help keep muscles strong.
Sometimes, therapists will use special machines to apply deep heat or electrical stimulation to reduce pain and improve joint movement.
Other therapies that may help ease joint pain include:
NUTRITION
Some people with RA may have intolerance or allergies to certain foods. A balanced nutritious diet is recommended. It may be helpful to eat foods rich in fish oils (omega-3 fatty acids). Smoking cigarettes should be stopped. Excessive alcohol should also be avoided.
More information and support for people with Rheumatoid arthritis and their families can be found by taking part in an arthritis support group.
Some people may benefit from taking part in an arthritis support group.
Whether your RA progresses or not depends on the severity of your symptoms and your response to treatment. It is important to start the treatment as soon as possible. Regular follow up visits with a rheumatologist are needed to adjust the treatment.
Permanent joint damage may occur without proper treatment. Early treatment with a three-medicine DMARD combination known as "triple therapy," or with the biologic or targeted synthetic medicines can prevent joint pain and damage.
If not well treated, RA can affect nearly every part of the body. Complications may include:
However, these complications can be avoided with proper treatment. The treatments for RA can also cause serious side effects. Talk to your provider about the possible side effects of treatment and what to do if they occur.
Contact your provider if you think you have symptoms of rheumatoid arthritis.
There is no known prevention. Smoking appears to worsen RA, so it is important to avoid tobacco. Proper early treatment can help prevent further joint damage.
Fraenkel L, Bathon JM, England BR, et al. 2021 American College of Rheumatology guideline for the treatment of rheumatoid arthritis. Arthritis Care Res (Hoboken). 2021;73(7):924-939. PMID: 34101387. pubmed.ncbi.nlm.nih.gov/34101387/.
McInnes I, O'Dell JR. Rheumatoid arthritis. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier; 2020:chap 248.
Mori S, Urata Y, Yoshitama T, Ueki Y. Tofacitinib versus tocilizumab in the treatment of biological-naïve or previous biological-failure patients with methotrexate-refractory active rheumatoid arthritis. RMD Open. 2021;7(2):e001601. PMID: 33958440. pubmed.ncbi.nlm.nih.gov/33958440/.
O'Dell JR. Treatment of rheumatoid arthritis. In: Firestein GS, Budd RC, Gabriel SE, Koretzky GA, McInnes IB, O’Dell JR, eds. Firestein & Kelley's Textbook of Rheumatology. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 77.
For generations, we have known that fruits and vegetables are good for our health. Multiple studies show time and again that we live longer when we eat more…

January 26, 2021
Combining an anti-inflammatory drug with an antiviral drug reduces recovery time and accelerates improvement for COVID-19 patients, a national study…
Department of Emergency Medicine, +3 more
If you’re a bricklayer or concrete worker, your job might be making you sick. A study of men in those fields showed they have an increased risk of developing rheumatoid arthritis through exposure...
Urinary tract infections are no fun, but new research shows they may have a silver lining. Along with infections in the gut and the genitals, U-T-I-s seemed to be linked with a lower incidence of...
Bottoms up, ladies? A newly published article on alcohol consumption and rheumatoid arthritis shows there may be a link between drinking alcoholic beverages and a reduced risk of R-A in women. The...