The Year in Review: Celebrating Our Achievements in 2017, Part 2
Part 2 of our “Year in Review” focuses on the hospitals, research institutes and centers that are part of the UF Health family:
- UF Health Cancer Center
- UF Clinical and Translational Science Institute
- UF Institute for Child Health Policy
- The UF Diabetes Institute
- UF Emerging Pathogens Institute
- UF Genetics Institute
- UF Institute on Aging
- Evelyn F. & William L. McKnight Brain Institute
- UF Health Shands
- UF Health Jacksonville

UF Health Cancer Center
Director: Jonathan D. Licht, M.D.
The University of Florida Health Cancer Center continues to grow and develop toward a submission for a Cancer Center Support Grant from the National Cancer Institute. Over the past year, all of the associate directors of the Cancer Center were named and members have been hard at work shaping our center. Research programs were firmly established, numerous recruitments finalized and metrics of collaboration, research funding and clinical research engagement are on the rise. Dr. Licht and the associate directors, program leaders and staff of the Cancer Center had a full-day strategic retreat in the summer of 2017 followed by weekly executive meetings of the associate directors to plan and implement the growth of the center. Monthly meetings with the program leaders and staff assure close communication and alignment of the center. The roles of the Cancer Center leadership and accomplishments this year are outlined below.
John Wingard, M.D., who also leads clinical research in hematopoietic stem cell transplantation in the Division of Hematology/Oncology, is the center’s deputy director. Dr. Wingard led a center-wide strategic planning process based upon surveys and focus groups with basic, clinical translation, population science-based researchers as well as clinical providers and community supporters. From this exercise, we developed our scientific programs, redesigned our system of clinical research management, organized our research education training programs and formulated an approach to community outreach.
Rolf Renne, Ph.D., an eminent virologist with an interest in Kaposi’s sarcoma virus-induced cancer became the associate director of basic sciences. Under his guidance, we have developed two laboratory-based research programs: Mechanisms of Oncogenesis, whose founding program leader was Dr. Robert Hromas, who has been appointed as dean at UT San Antonio. Dr. Renne will be the interim leader of this program, which has major themes in abnormal chromatin and gene regulation in cancer, the biology of RNA processing in cancer and tumor virology, the latter theme anchored by a new P01 grant led by Dr. Renne. The MOO program will be strengthened by the recruitment of Zhijian Qian, Ph.D., from the University of Illinois. Joining the Division of Hematology/Oncology of UF in March 2018, Dr. Qian is an expert in abnormal gene regulation in leukemia. Our other laboratory-based program is called Cancer Therapeutics and Host Response, co-led by Duane Mitchell, M.D., Ph.D., of neurosurgery, an expert in brain tumor-directed immunotherapy, and Christian Jobin, Ph.D., of the department of medicine, an international authority on the role of the microbiome in cancer. This program has major themes in immunotherapy, inflammation, immunity and the microbiome and small molecular anti-cancer therapeutics. This latter theme will be enhanced by the recruitment to the College of Pharmacy of Daohong Zhou, Ph.D., and Guagrong Zheng, Ph.D., from the University of Arkansas who will occupy newly constructed space in the Basic Sciences Building. These scientists team up to create novel anti-cancer agents that lead to the degradation and elimination of cancer-causing proteins.
This past fall, Dr. Renne and the Cancer Center led a major new initiative, inviting 10 of the most promising young postdoctoral fellows in the country who hold the NIH K99/R00 transitional grant to a research showcase forum in November 2017. During the showcase, these investigators, intermixed with newly recruited UFHCC K99/ROO holders Olga Gurynaova, M.D., Ph.D., and Mingie Xie, Ph.D., presented their research findings to a broad audience of Cancer Center members. These young investigators met with our faculty and toured the facilities across the University of Florida. Several of these investigators are now under active recruitment to assistant professor positions by the center.
Elizabeth Shenkman, R.N., Ph.D., also chair of the Department of Health Policy and Biomedical Informatics, was named associate director for population sciences. Under her guidance, the Cancer Population Sciences program was designed. The CPS program, co-led by Diana Wilke, R.N., Ph.D., of the College of Nursing, and Janice Krieger, Ph.D., of the College of Journalism, has major themes that include understanding and implanting strategies to improve communications and shared decision-making between cancer patients and caregivers and health systems. The program also advances symptom science and palliative care research, and multi-level interventions that address the social determinants of health and cancer health disparities. Through the One Florida Data Trust and other large data sets, the program elucidates emerging cancer health trends. Recruitments to augment the program this past year included Carma Bylund, Ph.D. (College of Journalism), a health communication expert; Russel Hemple, Ph.D. (College of Public Health and Health Professions), who studies cancer related muscle and soft tissue loss; and Stephen Huo, Ph.D., (College of Public Health and Health Professions) a health services researcher. Very notable this year was the award of a $12 million multi-site award from the PCORI (Patient-Centered Outcomes Research Institute) to Dr. Nancy Mendenhall to study patient-reported as well as objective outcomes from proton therapy.
Dr. Shenkman led an intensive study of the Cancer Center catchment area of 21 north central Florida counties using geographic and demographic information from the Florida Cancer Data System, random-digit dialing of households and information from one-on-one engagements by HealthStreet, a community engagement project also funded by the Cancer Center as well as the CTSI. The analysis so far shows our region to have high rates of smoking, obesity, poverty, impaired access to health care and modest health literacy. These findings are driving our strategy for Community Outreach and Engagement, a new and essential feature of NCI-designated cancer centers, and faculty and staff leadership for this office will soon be named.
Thomas George, M.D., was named associate director of clinical sciences and medical director of the Cancer Center’s clinical trials office. Dr. George, working closely with Alison Ivey, R.N., administrative director of the Cancer Center clinical trials office, and Dr. Brian Sevier, director of the UF Office of Clinical Research, has redesigned our Clinical Protocol Management System, an essential feature of every NCI-designated center. Dr. Sevier is working closely with Merry-Jennifer Markham, M.D. (Heme/Onc), associate director for clinical affairs, to created a dozen disease site groups, each with a clinical care and clinical research lead, covering tumor sites such as brain, breast, lung, blood and others. In addition, an early phase program called the Experimental Therapeutic Incubator was developed to facilitate clinical trials based upon cancer genetics and spanning multiple types of tumors. These groups originate clinical trial ideas and begin writing protocols with the help of the clinical trials office and medical writing, budgetary and regulatory staff. An example was the development of a phase I trial of PARP1 inhibitors in tumors with mutation of the BAP1 gene, based upon lab work from Dr. Hromas’ group. Carmen Allegra, M.D. (Heme/Onc), chief of the division of hematology/oncology and senior leader for clinical translation, has developed formal and informal training sessions to assist the translation of basic ideas into clinical protocols, this facilitated by his leadership role in the NCI Cancer Therapy Evaluation Program. Through Dr. Allegra and Dr. George’s efforts, the Cancer Center, through the University of Pittsburgh, became an affiliate member of the Experimental Therapeutics Clinical Trials Network, giving UF investigators access to a range of molecules being offered by the NCI for early phase clinical development.
Clinical trials are evaluated prospectively for scientific merit and priority to receive clinical trial office support by the Protocol Review and Monitoring Committee led by Paul Crispen, M.D. (Urology), consisting of members from a range of clinical disciplines. Trial conduct, patient safety and data integrity are managed by the Data Integrity and Safety Committee led by Dr. Wingard. Clinical trial accrual remains robust, with an increasing fraction of patients in investigator-initiated clinical trials. In addition, the center supported the development of a Good Manufacturing Process, or GMP, facility required for immunotherapy trials.
Steven Madore, Ph.D., associate director of the UF Interdisciplinary Center for Biotechnology Research, was named associate director for shared resources and core technologies to ensure harmonization of core technologies of the Cancer Center with UF at large. Working closely with Dr. Licht, Dr. Renne and other Ads, he is organizing the shared resources that will be supported by the Cancer Center Support Grant. These include Flow Cytometry and Microscopy, an Oncogenomics facility consisting of high-throughput DNA sequencing and bioinformatics and a newly designed Biostatistics Shared Resource, and a Drug Development shared resource. A developing core in gene editing CRISPR technologies was launched, led by Dr. Chris Vulpe (Veterinary Medicine). Plans are solidifying for a Biospecimens core to be developed in collaboration with the Clinical and Translational Sciences Institute and the Department of Pathology. Planning for a shared resource using mobile health and other electronic means to further populations sciences resource has begun as well.
Dietmar Siemann, Ph.D., was named associate director for cancer research career enhancement. Dr. Siemann has developed a set of programs develop the careers of aspiring cancer researchers. This includes participation in the pre-collegiate program in cooperation with local high schools, engagement of UF undergraduates in partnership with the UF Scholar program and the development of a Concentration in Cancer Biology in our academic health center’s Interdisciplinary Graduate Program, co-led by Maria Zajac-Kaye, Ph.D. (Cell Biology). The Cancer Center predoctoral award program helps fund cancer-focused Ph.D. students in the dissertation phase of their career. Dr. Siemann is developing a UFHCC Postdoctoral Cancer Research Fellowship Program to aggressively recruit postdoctoral fellows eligible for NIH funding. To develop junior faculty, the Cancer Center formed a partnership with the CTSI and funded several translational investigators through the KL2 program. Seminars in best practices in clinical research and a Translational Acceleration Program led by Drs. Allegra and Mitchell stimulate the development of investigator-initiated clinical trials. Folakemi Odedina, Ph.D., leads efforts in underrepresented minority engagement in cancer research through a P20 grant-funded Florida Minority Cancer Research & Training (MiCaRT) Center in partnership with Florida A&M, a historically black university. This year, Dr. Odedina was awarded a NCI R25 education grant titled “Comprehensive Research Training Opportunities for Outstanding Leaders” to provide research training of 11 underrepresented minority undergraduate and four underrepresented minority graduate students annually at UF and institutions in Africa, the Caribbean and Europe. Dr. Odedina is preparing a U54 application with FAMU and the University of Southern California to build upon the success of the MiCaRT Program.
Robert Houlihan, D.H.A., was recruited to the Cancer Center in early 2017 to become associate director for administration. Dr. Houlihan’s previous position was at the Virginia Commonwealth University, where he was the assistant director for administration of their NCI-designated center. Dr. Houlihan has organized the administrative staff into five major groups. These include Research Administration to support the three research programs, maintain and expand membership opportunities in the center and collect the data required for the Cancer Center Support Grant; Research Development to administer pilot bridge and selective submission grant opportunities; Administrative Services for recruitment, human resources, finance and budgeting; Marketing and Communication to promulgate clinical and research advances from the center; and Development to engage community supporters and philanthropy. Dr. Houlihan has engaged two former administrative directors of NCI-funded cancer centers to advise leadership on the structure and function of the UF Health Cancer Center. Our Cancer Center administration also organizes the yearly External Advisory Board meeting, to be held this year in March. The advice of this group of cancer center leaders and administrators will be critical as we formulate the submission of the Cancer Center Support Grant.
With a robust set of leaders, internal and external recruitment to the center, NCI and cancer-focused NIH funding of over $15 million per year, increasing translation of basic findings into clinical research, solid core facilities and exciting educational and community engagement programs in development, the we are now poised to develop a strong application to the National Cancer Institute. The writing of this document has begun, with submission anticipated in the spring of 2019.
Clinical and Translational Science Institute
Director: Dave Nelson, M.D.
Continuing to serve as a catalytic hub for translational research, the CTSI last year helped more than 1,300 investigators, graduate students, trainees and research professionals navigate the research landscape, find potential collaborators and access CTSI services. About 200 scientific publications were generated about research facilitated by CTSI resources.
In 2016, the CTSI developed a three-year strategic plan to operationalize five goals in pursuit of its mission. Highlighted accomplishments toward advancing each goal are summarized below. CTSI accomplishments reflect the dedication of hundreds of faculty, staff and students from across the university and at partners throughout the state.
Improving the UF Translational Research Environment
As research funding has grown across the institution, so has the research volume and sustainability of the CTSI’s Clinical Research Center, which has increased its active protocols from 82 in 2012 to 176 in late 2017, including 77 multisite studies involving other Clinical and Translational Science Award institutions. Outpatient visits increased from 2,446 to 4,208 in the same period.
In 2017, the CTSI expanded its institutionwide role in clinical research management and facilitation by completing Phase 1 of an enterprise-level OnCore clinical trials management system implementation and establishing a new Office of Clinical Research, with joint oversight by the CTSI and the UF Health Cancer Center.
The CTSI also launched a Translational Drug Development Core, and the Network Science Program led a novel, network-informed pilot intervention to foster team science.
Collaborating with the UF Informatics Institute, the CTSI launched a new pilot opportunity this spring as a result of a 2017 roundtable series that convened more than 70 translational thought leaders, methodologists and informaticians to discuss opportunities and challenges related to advanced data capabilities and methods development in translational health research.
Translational Workforce Training and Education
The CTSI Translational Workforce Development Program has taken a leadership role in reorganizing graduate, postgraduate and junior faculty development in clinical and translational science at UF. In 2017, the CTSI launched five of six career interest teams and supported more than 40 faculty members and trainees across its KL2, TL1, TRACTS and Mentor Academy programs. The TL1 Predoctoral Training Program appointed its first cohort composed exclusively of interdisciplinary trainee teams, and the Biomedical Informatics Program launched its Ph.D. program in the fall. The CTSI’s novel K College, T Team and F Force concepts have grown to convene more than 150 early-stage investigators as well as T and F directors and trainees across multiple colleges, thus enhancing support and creating a sense of community for scholars, trainees and mentors. New K Awards at UF have increased from seven in 2014 to 14 in 2016. Similarly, T32 Programs at UF have increased from nine in 2014 to 18 in 2017. In 2018, a new T32 postdoc training program will launch to support applied research and development in genomic medicine, developed by the CTSI’s Personalized Medicine and TWD programs.

Learning Health System Initiatives
The past year yielded progress in multiple areas designed to strengthen UF’s learning health system capacity:
Precision Medicine: The UF Health Personalized Medicine Program continued to develop, implement, study and refine methods that allow genetic information to be used as a routine part of patient care. CTSI resources facilitated an ongoing project at UF Health Jacksonville to study a point-of-care pharmacogenetics testing approach to guide clopidogrel therapy for heart stent patients, an IGNITE-funded project to study genomic-assisted proton pump inhibitor use in GI clinics, and two CTSI Translational Pilots.
Translational Pilots: CTSI supported five new projects through its NIH-funded Translational Pilot Program. In July, the CTSI’s Admin Core, Implementation Science Program and Personalized Medicine Program organized a retreat to develop recommendations for operationalizing a CTSI-facilitated process through which the UF Health research and clinical missions can come together to develop and vet learning health system collaborations, starting with 2018-19 Translational Pilots.
Clinical Informatics: CTSI and UF Health advanced a number of clinical informatics priorities, including three Epic/MyChart research projects; development of a plan and oversight committee for future Epic research builds; development of OnCore-Epic-REDCap-Vestigo interfaces; integration of patient-reported outcomes into the electronic health record (CTSA collaborative innovation award led by Northwestern); and deployment of CTS-IT’s open-source UF Health Quality Improvement Project Registry and CQI Approver (more than 500 users, and more than 250 projects registered to date).
Integrated Data Repository and Consent2Share: The UF Health Integrated Data Repository continued to expand, with 7,585 i2b2 queries in 2017 and data representing more than 1.5 million patients in Gainesville and Jacksonville. IDR data includes whether patients have agreed to participate in Consent2Share, which offers UF Health adult and pediatric patients an opportunity to allow UF researchers to contact them about research studies for which they might be eligible based on information in their electronic health record. Expansion is ongoing, with more than 47,000 patients enrolled to date.
Statewide and National Collaborations
CTSI made significant strides in expanding statewide and national collaborations to amplify the collective impact of translational research for the state and nation:
OneFlorida Clinical Research Consortium: UF CTSI joined the NIH All of Us Research program with a 2017 grant led by the University of Miami in collaboration with UF, Emory and Morehouse. As coordinating center for OneFlorida, CTSI bridges two national research networks — the CTSA consortium and PCORnet. To date, OneFlorida has supported 180 proposals and projects in the planning phase, with 40 applications awarded. In 2017, OneFlorida Data Trust expansion continued (15 million patients), with 126 queries fulfilled and OneFlorida i2b2 instances established.
Community Engagement: Celebrating its sixth year at UF, HealthStreet has enrolled more than 2,000 members in UF studies since 2011, the majority of whom are racial/ethnic minorities. In 2017, HealthStreet collaborated with 15 CTSAs to disseminate five national Our Community, Our Health town halls. In addition, the Citizen Scientist Program developed and launched a seven-module online curriculum as an Open Educational Resource in 2017.
Multisite Studies: A CTSI liaison team facilitated UF’s participation in the CTSA Trial Innovation Network, including the SMART IRB. In addition, FSU and six other OneFlorida partners joined the SMART IRB, and the OneFlorida IRB approved 20 studies in 2017. Multisite studies facilitated by the CTSI in 2017 include four CTSA Trial Innovation Network proposals; 22 active OneFlorida observational and interventional studies; and the $15 million WARRIOR trial (50 sites) led by Dr. Carl Pepine at UF and funded by the Department of Defense.


Institute for Child Health Policy
Director: Betsy A. Shenkman, Ph.D.
Equipped with new tools and technology and a strong research infrastructure, faculty and affiliates at UF’s Institute for Child Health Policy, or ICHP, led by Director Betsy Shenkman, Ph.D., continue to improve the health of children, adolescents and young adults nationwide through rigorous research and powerful research partnerships.
A new name for ICHP’s academic home
The College of Medicine’s department of health outcomes and policy, which serves as the academic home for many ICHP faculty, has changed its name to the department of health outcomes and biomedical informatics, or HOBI. Shenkman, who serves as chair of HOBI, said the name change reflects the growing importance of biomedical informatics in research. The biomedical informatics team is led by William Hogan, M.D., M.S., a professor of biomedical informatics in HOBI and director of biomedical informatics at the UF Clinical and Translational Science Institute.
The team now includes six faculty and an mHealth lab. Ongoing child health research involving biomedical informatics includes:
- Jiang Bian, Ph.D.; Yi Guo, Ph.D.; and François Modave, Ph.D., are investigating the feasibility of harnessing smart technology, including smartphones and smart wearables such as the Fitbit wristband, to help physicians monitor their adolescent patients with asthma.
- Modave is collaborating with the department of pediatrics to develop technology aimed at educating families and children newly diagnosed with diabetes about how to manage the disease.
- Stephanie Staras, Ph.D., whose National Cancer Institute-funded research focuses on improving teen compliance with the human papillomavirus, or HPV, vaccine using tablet-based health information technology, is investigating the best way to implement new technology in pediatric clinics by incorporating it into existing workflows.
- With more than $1 million in funding from the U.S. Department of Justice during the past three years, Chris Delcher, Ph.D., continues to help Florida law enforcement, state agencies and other stakeholders strengthen and refine Florida’s Prescription Drug Monitoring Program. In a separate study published last year in the American Journal of Public Health, Delcher and his team found that maternal and infant hospital stays associated with cocaine use fell almost immediately when in 2006 the federal government began regulating sodium permanganate, a key chemical needed to illegally manufacture cocaine.
- Mildred Maldonado-Molina, Ph.D., and UF’s Florida Data Center received a three-year, $540,000 funding award from Florida’s Agency for Health Care Administration to develop a statewide Child Care Access Index. The index, developed in collaboration with UF’s Lastinger Center and UF’s Anita Zucker Center for Excellence in Early Childhood Studies, will measure the extent to which quality child care is locally accessible in Florida. The program marks an important step in realizing the Florida Data Center’s long-term goal of linking education and health data for children in Florida.
Partners in research
The OneFlorida Clinical Research Consortium, where Shenkman serves as director and lead PI, has coalesced into a leading-edge resource for child health investigators at UF, in Florida and nationwide. The consortium’s Practice-Based Research Network brings together community-based practices, academic institutions and large health systems throughout urban and rural areas of Florida, which together provide health care to more than 40 percent of Floridians in the nation’s third-largest state. The OneFlorida Data Trust also houses robust patient-level electronic health record data, such as diagnoses, procedures, medications, patient demographics and other data elements for some 15 million Floridians, and includes data for all children enrolled in Medicaid in Florida. ICHP research supported by this infrastructure includes:
- QUALITY CHeQ: Shenkman, who is nationally renowned for her expertise in evaluating pediatric quality of care, received $675,000 in initial funding from the federal Agency for Healthcare Research and Quality, or AHRQ, and the Centers for Medicare and Medicaid to improve the usability of quality of care measures in diverse clinical settings. Shenkman and her team are evaluating two new quality measures developed by the AHRQ’s Pediatric Quality Measurement Program Centers of Excellence: preventive oral health care and safe and judicious use of antipsychotic medications in children and adolescents. UF is one of only six institutions nationwide to participate in the program.
- ICHP evaluates quality of care for children enrolled in Medicaid managed care programs in Texas and Florida. Nearly 1 in 5 children enrolled in Medicaid nationwide reside in Texas and Florida, the second- and third-largest states in the United States, respectively.
- Ramzi Salloum, Ph.D., is working with the OneFlorida Cancer Control Alliance to improve the capacity of pediatric clinics across Florida to screen and counsel their adolescent patients on tobacco use, using evidence-based approaches. Salloum implemented an adolescent tobacco intervention in MyChart, the Epic patient portal.
Leaders in service
ICHP faculty members continue to provide leadership, expertise and community service and outreach at the national, state and local level.
- Shenkman was appointed to serve on the PCORI executive committee and as co-chair of PCORI’s pediatric collaborative research group. Shenkman also accepted an appointment to serve as associate director for population sciences at the UF Health Cancer Center.
- ICHP Assistant Director of Clinical Research Lindsay Thompson, M.D., M.S., received the American Academy of Pediatrics’ 2017 Local Hero Award for her leadership, community action and advocacy for children in Gainesville and surrounding communities. Thompson, an associate professor of pediatrics and health policy at UF, is one of only two pediatricians in the United States and Canada to receive this prestigious award. Thompson is also spearheading a project to form a campuswide clinical research hub in the department of pediatrics.
- ICHP Associate Director Matthew Gurka, Ph.D., helped organize and host UF’s inaugural National Early Childhood Summit in Orlando last March. The summit, convened by UF’s Anita Zucker Center for Excellence in Early Childhood Studies and other colleges, centers and institutes across UF, brought together more than 100 scholars, policy makers, advocates, philanthropists and practitioners from around the country to create actionable ideas and steps to further early childhood development and learning. Gurka, a biostatistician with extensive collaborative and independent research experience in pediatrics, holds a joint faculty appointment with the Zucker Center.
- Ramzi Salloum, Ph.D., was selected to serve on the AAP’s Tobacco Consortium, which is responsible for setting a national agenda for child and adolescent tobacco prevention and cessation for the AAP’s Julius B. Richmond Center of Excellence. The center supports research and policy development aimed at protecting children from tobacco and secondhand smoke.
In 2017, ICHP leadership developed a recruitment campaign to expand its affiliate program, launched a new monthly newsletter (ICHP in a Minute) and booked Peter Margolis, M.D., Ph.D., a professor of pediatrics and co-director of the James M. Anderson Center for Health Systems Excellence at the Cincinnati Children’s Hospital Medical Center, to deliver the keynote presentation at ICHP’s 2018 Research Day on April 5.
In addition to providing a collaborative space and infrastructure for child health researchers across UF’s campus, the institute’s faculty members garnered $33,466,047 in total research funding in fiscal year 2016-17.
The UF Diabetes Institute
Director: Mark Atkinson, Ph.D.
The UF Diabetes Institute completed its third year in 2017, pushing forward toward its overarching mission to improve the lives of those living with diabetes so that we may one day see a diabetes-free world.
With one new person diagnosed with diabetes every 23 seconds and approximately one quarter of patients admitted to a UF Health Shands hospital having diabetes as part of their medical diagnosis, our mission is not only obvious … but increasingly urgent.
In picking one word to describe the Diabetes Institute for 2017, it would be that of growth. Indeed, this past year not only saw continued growth for some of UF’s hallmark diabetes programs but also marked expansion in many new areas not previously associated with our institute. While many notions could be highlighted, below are a represented selection from a program dedicated to research, improved patient care, training and public outreach — all efforts for which we at UF are proud to be a part.
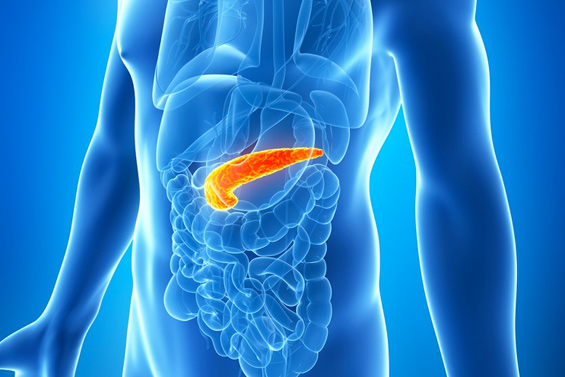
Research
Most people are aware of the importance of the heart, brain and lungs to healthy living, but the pancreas is one of the human body’s most often forgotten organs. That is, unless it isn’t working. The Diabetes Institute is helping to grow a strategic and highly collaborative effort focused on pancreas research at UF. So much so, we now think of ourselves as “Pancreas U.” Indeed, we have been the coordinating center for the JDRF’s Network for Pancreatic Organ donors with Diabetes (nPOD) program for a full decade ($26 million in funding to date); multiple Diabetes Institute investigators lead pancreas/pancreatic islet research programs funded by the National Institutes of Health, including those within the Human Islet Research Network, or HIRN; and the Leona M. and Harry B. Helmsley Charitable Trust is supporting a pioneering effort to create a Human Atlas of Neonatal Development & Early Life Pancreas, or HANDEL-P, to describe in detail how the pancreas develops from birth through 10 years of age, among other efforts. The Diabetes Institute is also overseeing a program that screens organ donors across the United States for blood-based biomarkers reflective of diabetes, among the largest non-transplant-related research efforts within the organ procurement organizations in the country.
Beyond increasing efforts in pancreas research, in both 2016 and 2017, we placed an emphasis on obtaining NIH grants dedicated to research training, and the results have been remarkably rewarding. These efforts are highlighted, below.
Additional examples of research and training notables in 2017 include:
- In December 2017, the Juvenile Diabetes Cure Alliance noted UF as the No. 3 entity in the United States receiving NIH funding for Type 1 diabetes.
- Drs. Asbhy Walker and Michael Haller received a $1.6 million grant from the Leona M. and Harry B. Helmsley Charitable Trust to pilot a program that will improve access to care for underserved adults and children living with diabetes. This grant is a collaborative effort with Stanford University; participating primary care providers in Florida and California will address urgent racial, socioeconomic and geographic disparities for people living with diabetes.
- Desmond Schatz, M.D., received a major grant from the Patient Centered Outcomes Research Institute to support the formation of pragmatic trials targeting obesity in the southeastern United States.
- Dr. Mark Atkinson received a new NIH award ($3.4 million) that, together with investigators at the University of Pennsylvania and Vanderbilt University, will identify organ donors suitable for research investigations by the HIRN network.
- The University of Florida remained the world’s top recipient of research funding from JDRF, which is the largest nongovernmental entity providing funds dedicated to Type 1 diabetes. Indeed, our university receives nearly 10 percent of the annual research funding from this international organization.
- Drs. Michael Haller and Todd Brusko are collaborating with Cord Blood Registry® (CBR®) on a potential clinical trial exploring the use of cord blood expanded autologous regulatory T cells as an immunotherapy in children with Type 1 diabetes.
- In late 2017, it was announced that the JDRF and Leona M. and Harry B. Helmsley Charitable Trust would renew funding for the aforementioned nPOD program for an additional five years ($16.4 million).
Clinical Care
Starting with adult diabetes, Dr. Kenneth Cusi, chief of the division of endocrinology, diabetes and metabolism in the UF College of Medicine Department of Medicine, has led the charge to continue to improve comprehensive diabetes care at UF Health. Dr. Cusi created (and since 2013, chaired) the Diabetes Care Task Force to coordinate efforts and educate housestaff, faculty and other health care providers about inpatient diabetes care. With more than 14,000 outpatient visits in 2017 (~65 percent with diabetes), the UF adult endocrinology and diabetes division continues to relentlessly grow and serves as a referral center to the community and region (e.g., a 4-fold growth in outpatient visits in the past five years). Moreover, the division provided 5,120 inpatient consults and follow-up visits at UF Health Shands Hospital in 2017, and was recognized as offering the best inpatient consult service in 2015-2016, second best in 2017, by physicians within the UF Department of Medicine.
- With 21 endocrinologists and advanced registered nurse practitioners, the UFDI hosts the second-largest regional endocrine, diabetes and metabolism program (after the University of Miami).
- In the 2016-17 U.S. News & World Report rankings, UF ranked 31st among national adult endocrine programs (second in the state of Florida).
- The UF adult endocrinology & diabetes division ranked second across the department of medicine, after nephrology.
- More than 10 randomized control trials and research studies are ongoing in Type 2 diabetes, obesity and nonalcoholic fatty liver disease. Having developed state-of-the-art stable isotope and liver imaging techniques, UF hosts one of the leading clinical translational research programs in the United States in Type 2 diabetes and nonalcoholic fatty liver disease.
- Recently reported in the Annals of Internal Medicine (the official Journal of the American College of Physicians), findings from a three-year clinical trial led by Dr. Kenneth Cusi revealed that the drug pioglitazone is the first safe and effective intervention for patients with prediabetes or Type 2 diabetes who have nonalcoholic steatohepatitis, a chronic liver disease caused by fat buildup in the liver that is the second cause of cirrhosis in the United States. Indeed, fatty liver disease is a risk factor for Type 2 diabetes, even in non-obese patients.
The pediatric endocrinology and diabetes program, led by Michael Haller, M.D., was ranked 23rd in pediatric endocrinology by U.S. News & World Report, and our pediatric endocrinology division received the Most Outstanding Division Award for the department of pediatrics for the fourth consecutive year. The pediatric diabetes faculty sees over 1,000 unique diabetes patients per year and continues to offer leading-edge care to children and families affected by diabetes. The Florida Diabetes camps, directed by UF pediatric diabetes faculty, also served over 500 children with diabetes in 2017.
- The pediatric endocrinology group now boasts eight M.D. faculty, two ARNPs, four certified diabetes educators, two registered dietitians and psychology support embedded in our clinics. We offer diabetes education five days per week as well as evening classes in advanced diabetes pumping and continuous glucose monitoring.
- The UF pediatric diabetes program was chosen as one of only four sites internationally to test the Medtronic 690G artificial pancreas system.
- The UF Pediatric Diabetes Program played an integral role in the studies that led to the recent acquisition of intranasal glucagon by Eli Lilly and Company.
- Our Pediatric Fun and Fit program, led by Dr. Angelina Bernier, has demonstrated reductions in BMI percentile in our overweight youth.
- Drs. Martha Campbell-Thompson and Michael Haller completed their NIH-funded DP3 demonstrating reduced pancreas volume in children at risk for developing Type 1 diabetes.
- Dr. Michael Haller led the NIH TrialNet consortium in reaching the primary outcome in a randomized clinical trial of ATG and GCSF in new-onset Type 1 diabetes patients (manuscript under review at The New England Journal of Medicine).
- Dr. Arlan Rosenbloom received the Judson VanWyk Award, the highest award bestowed by the Pediatric Endocrine Society.
Training
As mentioned previously, with an interest in increasing training opportunities through obtaining funding, we note a newly funded interdisciplinary T32 Training Grant bridging the studies of diabetes and biomedical engineering (led by Drs. Mark Atkinson and Dr. Ben Keselowsky) along with other Diabetes Institute members (Drs. Todd Brusko, Michael Clare-Salzler, Patrick Concannon, John Driver, Clayton Mathews, Michael Haller, Gregory Hudalla, Lyle Moldawer, Laurence Morel, Desmond Schatz, Janet Silverstein, Cherie Stabler, Mark Wallet, Shannon Wallet and Lin Yang). Diabetes Institute-supported trainees also saw an remarkable of accomplishment, examples including two pre-doctoral students (Ms. Olivia Bailey and Ms. Melanie Shapiro) receiving NIH F31 (diversity) awards and third-year pediatric endocrine fellows (Dr. Kristen Dayton and Dr. Laura Jacobson) receiving highly competitive extramural grants from the Pediatric Endocrine Society and the JDRF, respectively.
With six physicians-in-training in the Adult Endocrinology Fellowship program, UF is the second-largest adult endocrine training program in the state of Florida. The program, which provides leading-edge diabetes care training to fellows with the latest on insulin pump + continuous glucose monitoring outpatient care technology, receives more than 160 applications for endocrinology fellowship training each year. Moreover, UF has regional leadership in subspecialty and multidisciplinary endocrine care clinics for patients with thyroid cancer, pituitary disease, lipid management, cystic fibrosis, obesity medicine program, nonalcoholic fatty liver disease, osteoporosis and more. UF endocrinology division faculty members hold leadership roles in national medical societies in education and research, including the ADA, the Obesity Society and the Endocrine Society. Over 30 peer-reviewed manuscripts were published by adult endocrinology trainees in 2017 alone (over 100 manuscripts published in the past five years).
UF’s pediatric diabetes and endocrinology division has three fellows, two of which are graduating in 2018 and will, as a sign of growth, remain as new faculty. These fellowships are quite competitive, with over 30 applicants turned down each year. In 2017, UF clinical fellows published over 20 manuscripts and, to varying degrees, participated in more than 50 ongoing clinical trials occurring within the division.
Outreach and Community Involvement
Here, the Diabetes Institute seeks to extend the mission to the community at large. For example, Dr. Anastasia Albanese-O’Neill in the UF Division of Pediatric Endocrinology serves as the co-chair of the American Diabetes Association’s Safe at School Working Group. The group works to make sure the diabetes management needs of students across the United States are met so these children are healthy and safe when they are at school and school-sponsored activities.
The Diabetes Institute now provides a variety of educational offerings in the use of diabetes technology, including an introductory class on diabetes technology, insulin pump training (start and advanced), continuous glucose monitoring training, and training on data transfer and interpretation. Patients and their family members have the option to participate in diabetes technology education in person, in a group setting, or via telehealth using Vidyo software. This latter program was made possible through a grant from the UF Children’s Miracle Network.
- The NIH-supported T1D DATA (Type 1 Diabetes Data Acquisition and Transfer Adherence) Study was undertaken at UF to improve glycemic control by facilitating data sharing of blood glucose, continuous glucose monitoring and pump data by patients between clinic visits.
- UF is one of 14 sites that participate in the SENCE (Strategies to Enhance New CGM use in Early Childhood) Study, examining the benefits of continuous glucose monitoring and continuous glucose monitoring + behavioral training in children ages 2-7 years with Type 1 diabetes. An added benefit of this study is that it has provided continuous glucose monitoring technology to many families who may not have otherwise been able to afford the device.
- In August, the Diabetes Institute hosted the Basketball Training Camp for former UF basketball player Corey Brewer. Corey, currently the NBA’s “Iron Man” for the longest number of consecutive games played, donates the proceeds from the camp to support diabetes care and education for underserved populations.

- Using continuous glucose monitoring, blood glucose and insulin pump data, this study pits the DreaMed Advice4U pro algorithm against medically guided recommendations by physicians to determine insulin dosing for suboptimally controlled patients with Type 1 diabetes, somewhat akin to “IBM’s Deep Blue versus the world chess champion Garry Kasparov.”
- Our Telehealth Transition Study provided group diabetes education via videoconference (Vidyo) for young adults (ages 18-25 years) with Type 1 diabetes who were transitioning to living away from home. The study had a companion website, where additional information on a variety of topics could be found. Links were pushed to participants immediately after each videoconference, with pronounced improvements in care observed.
- The Diabetes Institute was selected as one of six sites participating in the national Young Adult Racial Disparities in Diabetes, or YARDD study. Dr. Ashby Walker, our site PI, is collaborating with Dr. Shivani Agarwal at the University of Pennsylvania. The study seeks to better explicate the role of adverse childhood events in racial disparities for Type 1 diabetes.
- The Diabetes Institute spearheaded a number of exciting new initiatives for our college students with Type 1 Diabetes. Drs. Ashby Walker and Desmond Schatz successfully piloted the All for ONE mentoring program with grant funding from the Type 1 Exchange. This program paired college students living with Type 1 diabetes as mentors with publicly insured teens who also have Type 1 diabetes in the clinics at UF and is gaining national recognition for its innovation. As part of this program, 22 college students with Type 1 diabetes were able to participate in a directed research experience exposing them to the major research labs at the institute and related career trajectories. We also are providing support for the College Diabetes Network chapter on campus — a vibrant student group hosting monthly gatherings and many social network opportunities for college students with Type 1 diabetes.
- Dr. Lisa Scarton, of the UF College of Nursing, hosted a significant three-day conference in Gainesville, bringing in investigators (epidemiologists, health care providers, public health department heads) and tribal leaders from Native American Indian Tribes throughout the United States, for the purpose of identifying pragmatic ways of averting obesity in Native American families.
- On Nov. 14, 2017 the Diabetes Institute hosted an event for World Diabetes Day about “Women, Diabetes, and Health Equity.” This multi-college and multidisciplinary event showcased research about Type 1 diabetes and Type 2 diabetes in women’s health and was a tremendous success, including an opening proclamation of World Diabetes Day by Gainesville Mayor Lauren Poe.

Emerging Pathogens Institute
Director: J. Glenn Morris, M.D.
The Emerging Pathogens Institute continues to maintain a strong multidisciplinary research program, focusing on new and emerging pathogenic microorganisms causing disease in humans, animals and plants. In 2016, EPI played a major role nationally and internationally in work with the Zika virus, including reporting of some of the earliest Zika isolations in the hemisphere associated with study sites in Haiti. The year 2017 saw a rapid decline in Zika case numbers in Florida, the Caribbean and South and Central America, as the epidemic “burned out.” However, EPI investigators have continued to be actively engaged in work with Zika, as well as other arboviruses known to circulate in the region. Meanwhile, the global reach of the institute continues to expand, with EPI members collaborating on projects in over 75 countries, studying malaria, dengue, cholera, brucellosis, Xanthomonas infections, lymphatic filariasis and many other emerging pathogens that affect the health of people, plants and animals around the world.
Research Areas of Note
 Arboviruses: Five researchers at the University of Florida received nearly $3 million from the Florida Department of Health as part of its Zika Research Grant Initiative. EPI took an active role in the project proposals, both spearheading projects and collaborating with faculty members on research aimed at protecting Floridians from the virus. The institute was also the recipient of legislative funding through the State University System of Florida meant to further enhance EPI facilities for work with Zika and other arboviruses. Dr. Derek Cummings (CLAS) contributed to a Nature article finding that transmission of Zika virus in Florida was linked to travel from the Caribbean, along with an article in Science showing that the majority of dengue virus infections take place close to the home of the host and are transmitted by the same family of mosquitoes. Drs. John Lednicky, (PHHP) and Marco Salemi (COM) were responsible for a series of papers assessing evolution and transmission of Zika, Chikungunya, Mayaro, dengue and other viral pathogens; Dr. Sadie Ryan (CLAS) published research finding that temperature influences the transmissibility of arboviruses such as Zika, Chikungunya and dengue.
Arboviruses: Five researchers at the University of Florida received nearly $3 million from the Florida Department of Health as part of its Zika Research Grant Initiative. EPI took an active role in the project proposals, both spearheading projects and collaborating with faculty members on research aimed at protecting Floridians from the virus. The institute was also the recipient of legislative funding through the State University System of Florida meant to further enhance EPI facilities for work with Zika and other arboviruses. Dr. Derek Cummings (CLAS) contributed to a Nature article finding that transmission of Zika virus in Florida was linked to travel from the Caribbean, along with an article in Science showing that the majority of dengue virus infections take place close to the home of the host and are transmitted by the same family of mosquitoes. Drs. John Lednicky, (PHHP) and Marco Salemi (COM) were responsible for a series of papers assessing evolution and transmission of Zika, Chikungunya, Mayaro, dengue and other viral pathogens; Dr. Sadie Ryan (CLAS) published research finding that temperature influences the transmissibility of arboviruses such as Zika, Chikungunya and dengue.- Cholera and enteric diseases: Studies continued in Haiti, Bangladesh and Democratic Republic of the Congo. Dr. Ira Longini (PHHP/COM) published models showing that targeted use of oral cholera vaccines have the potential to end cholera transmission in Haiti. Drs. Glenn Morris (COM) and Afsar Ali (PHHP) were involved with a project, published in Nature Microbiology, finding that quorum sensing among Vibrio cholerae keeps cholera infection from becoming lethal to the host in arthropod models.
- Infant sepsis: Drs. Morris and Judy Johnson (COM) contributed to a project in India finding that giving newborn children at risk of developing sepsis Lactobacillus plantarum, a low-cost probiotic, may significantly reduce their chance of becoming infected; results were published in Nature.
- Animal Diseases: Drs. Samantha Wisely (IFAS) and Jason Blackburn continue to be active in the UF Cervidae Health Research Initiative (CHeRI), working to understand transmission dynamics of orbiviruses and other pathogens in farmed and wild deer (see photo).
Outreach

- In 2017, EPI hosted its largest-ever Research Day, with over 400 people registering to see nearly 150 poster presentations. Drs. Bill Pape and Marc Eloit delivered the keynote addresses. Dr. Pape spoke about GHESKIO, a Haitian health organization that was instrumental in the effort to slow the spread of HIV and tuberculosis in Haiti. Dr. Eloit, who leads the Pathogen Discovery Laboratory at Institut Pasteur, discussed animal viruses that pass into human populations.
- Several EPI members took part in CATALySES, a two-week program for science teachers aimed at introducing high school science teachers to the latest research in emerging pathogens and giving them the tools to incorporate this knowledge into their lesson plans. During the school year, teachers can visit campus labs with their students and gain access to an equipment locker, supplying them with lab equipment that would otherwise be unavailable to them.
- The Emerging Pathogens Institute sponsored the inaugural Haiti Water Summit at the State University School of Medicine in Port-au-Prince, Haiti. Several UF professors were featured in the program, including Dr. Tom Frazer, director of the school of natural resources and environment; Dr. Mary Jane Angelo, a professor of law and director of the environmental and land use law program; Dr. Wendy Graham, director of the University of Florida Water Institute; Dr. Eric Nelson, a pediatrician and member of the Emerging Pathogens Institute; and Dr. J. Glenn Morris, director of the Emerging Pathogens Institute. Dr. Nelson spoke on a “One Health” panel about how a smartphone application can help train first responders to outbreaks of waterborne diseases like cholera. He also led a workshop with professor Elda Déronette from the State University of Haiti about how consumer technology can help improve water security. During Dr. Morris’ section of the One Health panel, he discussed EPI’s research on the transmission of waterborne pathogens in Haiti.
- Moving forward into 2018, EPI will maintain its strong global research focus, with an interdisciplinary approach that incorporates human, veterinary and plant medicine, and makes use of leading-edge technology in genetics, microbiology, epidemiology, medical geography and mathematical modeling to understand new and emerging diseases.

UF Genetics Institute
Director: Patrick Concannon, Ph.D.
In 2017, the Genetics Institute welcomed six new faculty members from five different colleges of the University of Florida. The 220-member faculty of the Genetics Institute now represent seven colleges and 51 academic departments as well as the Marston Science Library, Health Science Center Library and Florida Museum of Natural History. During 2017, institute investigators secured $63 million in sponsored research support, filed 48 U.S. patents and published 771 scholarly articles. Their work appeared in a diverse array of prestigious journals, including The Journal of the American Medical Association, Science, Cell, and Nature Genetics and Nature Nanotechnology.
Mission
The aim of the UF Genetics Institute is to promote excellence in the areas of genetics and genomics by: (1) building community, facilitating collaboration and creating opportunities for intellectual exchanges among investigators working in diverse taxonomic systems but with a common set of approaches in genetics and genomics; (2) supporting recruitment and retention of outstanding faculty in the areas of genetic and genomics; (3) supporting graduate education in the areas of genetics and genomics; and (4) enhancing the ability of UF researchers to compete for multidisciplinary research grants in the area of genetics and genomics.
In 2017, the Genetics Institute initiated a pilot grant program offering early support for multidisciplinary research initiatives that had the potential to mature into projects that would compete effectively for extramural funding. Three pilot grant awards were made to institute members representing three different colleges and the UF Whitney Laboratory for Marine Biosciences.
Education
In 2017, the Genetics & Genomics Graduate Program, directed by the Genetics Institute, had 28 students training in 11 different departments in four colleges. Last year saw four G&G students earn their doctoral degrees, bringing the total number of graduates from the program to 27. This intercollegiate program continues to grow, with four more students admitted in the current year and interviews already underway for the class of 2018. Last year the Kenneth and Laura Berns Award for Excellence in Genetics, awarded annually for outstanding scientific contribution by a G&G student, went to Yong Shen, who is training in the laboratory of institute member Jorg Bungert.
Honors
In 2017, Doug Soltis, Distinguished Professor in the Florida Museum of Natural History, institute member and co-director of our Genetics & Genomics Graduate Program, was inducted into the prestigious National Academy of Sciences. He joins institute faculty members Harry Klee, Robert Cousins, Ken Berns and Pam Soltis, who also have received this honor.
Four Genetics Institute members were cited as being among the top 1 percent of most highly cited researchers worldwide over the last 10 years by Clarivate Analytics.
Outreach
The 2017 program of our annual cornerstone event, The Florida Genetics Symposium, was the most successful yet. Taking place Oct. 25–26, more than 550 people registered to attend — the most participants in the history of the event. The conference featured 12 distinguished speakers from UF and other institutions. Approximately 100 posters were presented, with student and postdoctoral associates receiving awards for best poster presentations.

In 2017, the institute’s weekly seminar series continued with internal and external speaker presentations. The invited speakers reflect our broad, multidisciplinary mandate. The seminars included outstanding investigators from the fields of bioinformatics, genomics and cell biology working on a variety of different species and model systems.

Institute on Aging
Director: Marco Pahor, M.D.
In 2017 our enterprise has continued to expand, capitalizing on the remarkable successes of the previous years in the areas of research, health care and education. The Institute on Aging has supported 49 extramural grants through cores, pilots and mentoring, with a total cost of $196 million, and $28 million in the 2017 annual period, which include major center grants, such as the Pepper Center, the P50 Sepsis project and the IOA contribution to the CTSI KL2 program, as well as large NIH-funded multicenter clinical trials and infrastructure grants, including the LIFE study, ASPREE, ENRGISE, MOTRPAC and the newly awarded JAX-ASCENT described below.
Research
JAX-ASCENT (total cost $3.76 million, Pahor and Anton PIs). Older adults of racial minorities and low socioeconomic status represent particularly high-risk populations who are underserved and are significantly underrepresented in clinical research. This has led to a gap in knowledge regarding the appropriate and/or optimal prevention and treatment approaches for this high-risk group. Within the state of Florida, the city of Jacksonville has a high proportion of minority and low socioeconomic status individuals. By expanding existing research collaborations on both aging and health disparities at its Jacksonville site, the University of Florida has a unique opportunity to conduct important research that can reduce this knowledge gap. These existing relationships include partnership in conducting multicenter NIH-funded clinical trials, along with several community outreach efforts at UF Health’s Gainesville and Jacksonville campuses. However, there is currently no cohesive, organized resource to integrate these important research collaborations in aging and health disparities at UF in Jacksonville.
At the Gainesville campus, we have a strong clinical translational research infrastructure with the Claude D. Pepper Older Americans Independence Center, the Clinical and Translational Science Institute, and Disparities Research. In Jacksonville, UF has a large health care facility in a densely populated minority and low socioeconomic status area, but limited research infrastructure focused on aging research. To fully actualize the potential of this remarkable resource, we develop a dedicated center for aging research focused on racial minorities and low socioeconomic status older adults. This state-of-the-art clinical translational research facility for multidisciplinary research — Jacksonville Aging Studies CENTer, or JAX-ASCENT — closely partners with the Gainesville campus and capitalizes on our expertise and resources. Additionally, JAX-ASCENT creates an integrative physical and intellectual environment in which trainees at all levels and scientists from diverse disciplines can interact and conduct clinical and behavioral translational research on aging and independence of older adults. This focus is pursued using an interdisciplinary approach that traverses a broad spectrum of biomedical investigation, including clinical research, behavioral sciences, social sciences, epidemiology, biostatistics and health services, while implementing rigor and transparency in research.
We develop and partner regarding expertise on clinical trials, recruitment, adherence, retention, assessment of geriatric outcomes, biomarkers and behavioral studies all focused and tailored on research in urban minorities and low socioeconomic status older adults. We apply a conceptual/logic model of community-based participatory research partnerships to improve community involvement and health outcomes, and to build a research participants registry. We develop the physical and human infrastructure, mentor junior faculty toward leadership roles, and have JAX-ASCENT become self-sustaining. JAX-ASCENT expands knowledge in clinical translational research in largely understudied populations and both enlarges and enriches the diversity of research in older minority populations, clinical effectiveness, outcomes and community engagement programs at UF.
With the development of JAX-ASCENT, we will provide resources and personnel (including NIH funded investigators) to support the development and implementation of behavioral, nutritional, and pharmacologic clinical trials, and observational studies of social determinants of health contributing to chronic diseases and functional decline in underserved, minority and low socioeconomic status older adults.
JAX-ASCENT will fill a critical gap in knowledge regarding the translation and dissemination of research from efficacy studies to underserved, minority older adults who are at high risk of geriatric conditions.
The LIFE study continues to be highly productive in data analyses and publications, with over 90 papers published in peer\-reviewed journals. The LIFE study has shared study materials, including protocols, manual of operations and procedures, and recruitment and retention materials, with 125 investigators and has involved over 900 investigators and staff members across over 20 institutions.
The NIH Pepper Older Americans Independence Center has been renewed through 2022 (total cost $5.1 million, Pahor, PI). That’s the third renewal of the UF Pepper Center in a row awarded at the first submission, demonstrating the continued high productivity of the center and department, and the Institute on Aging as a whole.
The ENRGISE pilot study (total cost $5.3 million, Pahor, PI) to assess the effects of fish oil and losartan on inflammation and mobility in older persons successfully completed recruitment of 290 participants at five sites.
The MoTrPAC Consortium Coordinating Center grant funded (total cost $9.3 million, Pahor, PI) to assess the Molecular Transducers of Physical Activity has just completed the first year of planning.
The PCORI Weight Loss among Obese Black Women (total cost $2.1 million, Anton & Tucker, PIs) has just been funded.
The IOA has a very rich pipeline of 22 pending grants ($30 million), and has produced a high return on investment of $8.69 in extramural funding per dollar invested in research and indirect cost return of $242 per square foot of research lab space.
Health Care
Our clinical practice (division chief, Dr. Solberg) experienced a superb year of growth and expansion with the restructuring of the division, introducing sections of Ambulatory Care, Acute Care, Post-Acute Care and Clinical Education. In the Ambulatory Care section, led by Dr. Susan Schneider, the division increased the availability of outpatient appointments when it hired additional geriatricians to provide care in our Senior Care clinic in the Clinical and Translational Research Building (IOA) and at Oak Hammock. Our practice providers and staff offered excellent care to our patients; our patient satisfaction survey results were in the highest quartile.
The Acute Care section, led by Dr. Jacobo Hincapie, increased the presence of geriatric medicine in the hospital. We continued to be active in ER consults to intervene early in the care of our older adults. We added an ARNP to the Geriatrics Consult Service team, enabling a consulting team that includes a geriatrician and ARNP to provide surgical and medical services in the hospital with a geriatrics focus in their care. Our model of the embedded geriatrician continues to show positive impact on inpatient outcomes.
In the fall, we opened the Acute Care for the Elderly, or ACE, Unit on unit 74 in UF Health Shands Hospital in partnership with the division of hospital medicine. The ACE unit adds a geriatrician-led interdisciplinary team that reviews all patients on the unit older than 70 years, imparting a geriatrics-focused care plan and management from the day of admission to discharge. The goal is to reduce length of stay, readmission rates and cost of hospitalization.
There was considerable expansion and growth in the Post-Acute Care section, led by Dr. Bhanuprasad Sandesara, through the partnerships forged this year between UF Health and two additional skilled nursing facilities and long-term care centers in the community. This brings the number of Post-Acute Care centers our division serves to four. Through these partnerships, we have increased the number of short-term rehabilitation beds available in the Gainesville community to UF Health patients. At these facilities, our embedded geriatricians and physician extenders work as a team on site every weekday. This helps shape our continuum of care, as it allows greater involvement in the care of the patient during rehabilitation, and our increased presence in the facility means fewer readmissions to the hospital. Additionally, we are improving the continuity of care we provide from the hospital to post-acute care, as our Geriatrics Consult Service team communicates directly with our Post-Acute Care section team. This seamless communication aids in the coordination of care, and thus the recovery and return to independence of our patients. The careful coordination of care among our division’s section enables our providers to focus patient care from clinic to hospital to rehabilitation and back to our practice, all under the care of a geriatrician.
Additionally, the geriatric medicine division continues to achieve its mission to support the department’s clinical research enterprise. Our physicians are active members of various department research study teams who interact with participants and promote discovery and innovation from a research as well as clinical perspective.
With our growth and increasing recognition on a national basis, UF Health Geriatric Medicine was again recognized by U.S. News & World Report, with the division ranking in the top 50 hospitals for geriatric medicine for 2017-2018.
Education
Medical Education. The restructuring of the division of geriatric medicine included the creation of a Clinical Education section, led by Dr. Mallory Otto. This section oversees our fourth-year medical student clerkship; this clerkship is mandatory for all medical students and teaches them about the unique aspects of geriatric medicine. We continued revising and improving the student experience and added a Humanism in Medicine week to the clerkship. Medical students learn to take an oral history by interviewing an older adult. The students then put together a video presentation video about the older adult they interviewed. These are archived in the UF Library as part of the UF Oral History Project. This year, the students continued their rotations on the clerkship in geriatric medicine, palliative care and rehabilitation medicine, and continued to complete simulations exercises to learn about polypharmacy and dementia.
Our Geriatric Medicine fellowship underwent a complete revision and redirection, with a new curriculum focused on the geriatric care environments and partnerships we have cultivated in the UF Health system. The fellowship is now based predominantly in the UF Health facilities and clinical sites, with our geriatrics faculty leading the way in teaching clinical geriatrics care. We maintain our commitment to the Veterans Administration Health System with rotations at the VA hospital with an innovative delirium consult team, palliative care, and the geropsychiatry program. With our newly revised and innovative clinical experience, our fellowship is growing in popularity and for the coming year our recruiting season was extremely successful, filling all four slots with fellows for 2018-2019.
Another successful innovation was our community education series of “Lemonade Chats” with a geriatrician, which were held at the Alachua County Senior Center. These informal discussion groups allowed older adults to learn about a particular topic and then discuss their own concerns with the geriatrician while enjoying a cool cup of lemonade. We will continue these well-received events every two months throughout the year.
Graduate Education. (committee chair, Dr. Carter) The UF IOA offers an online master’s degree in gerontology or graduate certificate in aging and geriatric practice. We offer 10 courses that address the basic biology of aging, geriatrics and age-related diseases, clinical neuroscience and the basics of research and epidemiology. We currently have 25 students enrolled in the online master’s program and 10 in the certificate program. Enrollees are professionals working in a variety of fields, including physicians, nurses, psychologists, directors of assisted living facilities, law enforcement officials, funeral home directors and policy makers.

Evelyn F. & William L. McKnight Brain Institute
Executive Director: Todd E. Golde, M.D., Ph.D. Deputy Director: Steven T. DeKosky, M.D.
The Evelyn F. and William L. McKnight Brain Institute continues to thrive at the University of Florida, and we are proud of the role that the MBI has in neuromedicine and neuroscience research. As of January 2018, active neuroscience- and neuromedicine-based NIH funding totaled approximately $58 million per year, with more than 90 researchers receiving NIH funding. This figure represents almost a quarter of all NIH funding that UF receives. Not only is the research project grant (R01) base growing with 66 active R01s, but an increased number of both programmatic and training grants have been awarded to UF faculty. UF neuroscience investigators are PIs on five neuroscience-related training grants (T32), as well as three collaborative research grants (U01), a program project grant (P01), a single-component research award (OT2) and a P50 award. Our trainees and junior faculty are gaining federal funding, with five fellowship awards (F grants), 11 career development awards (K awards) and four research transition awards (R00).
Grants from other federal agencies and private foundations also support UF neuroscience research. Two large, notable awards in 2017 came from the U.S. Defense Department under the Targeted Neuroplasticity Training program of the Defense Advanced Research Projects Agency, or DARPA. The first, a $4.2 million grant led by Kevin J. Otto, Ph.D., an associate professor in the J. Crayton Pruitt Family Department of Biomedical Engineering, will identify which neural pathways in the brain are involved in plasticity due to vagal nerve stimulation during learning. A second DARPA award, led by Karim Oweiss, Ph.D., a professor of electrical and computer engineering, biomedical engineering and neuroscience, seeks to determine effects of vagal nerve stimulation on cognitive-skill learning and the brain activity supporting those skills, as well as to optimize the stimulation parameters and training protocols for long-term retention of those skills.

Research in brain aging, neurodegeneration, neuromuscular pathophysiology, control of breathing, addiction, pain, gene therapy for central nervous system disorders, sensory physiology and neurooncology all have garnered national, and in many cases, international recognition. As the individual neuroscience and neuromedicine research programs mature, we are beginning to see more thematically oriented research, with more cross-disciplinary studies. This is leading to increasing numbers of larger multi-principal investigator R01 grants, P grants and U grants, as well as other large collaborative grants.
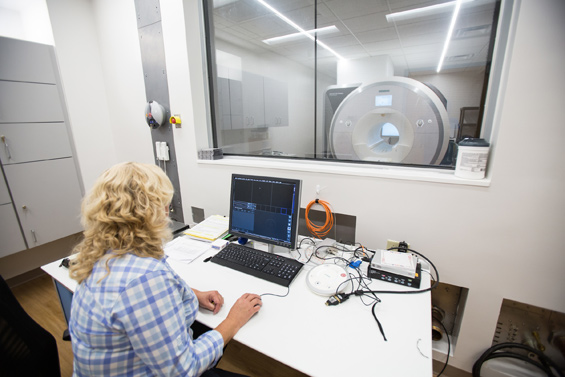
The MBI also made significant infrastructure upgrades to support human-subject-oriented research in 2017. A new 3T Siemens Prisma scanner dedicated to research studies was installed and has been available for scans since spring of 2017. Joanna Long, Ph.D., director of the Advanced Magnetic Resonance Imaging and Spectroscopy Facility, or AMRIS, and a professor of biochemistry and molecular biology, and her colleagues played a key role in obtaining this instrument with a $2 million shared instrument grant awarded by the NIH. A large room adjacent to the new scanner was renovated to provide additional multi-user, clinical research space so that pre- and post-scanning testing can be conducted easily. These pre- and post-testing rooms are available to all UF investigators using the AMRIS facility and can be scheduled at http://amris.mbi.ufl.edu/reservations/make-a-reservation/. These upgrades have already made a big impact at UF, supporting numerous grants. Such grants include:
- The Adolescent Brain Cognitive Development, or ABCD, study, a large, NIH-funded, multi-institution longitudinal study. UF site leaders are Linda Cottler, Ph.D., M.P.H., chair of epidemiology, and Sara Jo Nixon, Ph.D., a professor of psychiatry and psychology.
- Several muscular dystrophy imaging studies led by Krista Vandenborne, Ph.D., P.T., chair of physical therapy, including her research funded by a large NIH R01 titled “Magnetic Resonance Imaging and Biomarkers for Muscular Dystrophy.”
- Multiple grants centered on imaging of movement disorders, including a large U01 grant led by David Vaillancourt, a professor of applied physiology and kinesiology. In addition, the MBI partly supported the purchase of a light sheet microscope, which was funded primarily by the DARPA award to Dr. Otto.
Over the last year, the MBI changed its leadership structure to reflect the programmatic nature of our research and ensure that our education and outreach efforts are supported. In addition to Drs. Golde and DeKosky, the executive committee now includes:
- Jennifer Bizon, Ph.D., a professor of neuroscience, associate chair of neuroscience and member of the Age-Related Memory Loss program
- David Borchelt, Ph.D., a professor of neuroscience and director of the Center for Translational Research in Neurodegenerative Disease
- Ronald Cohen, Ph.D., a professor of clinical and health psychology, neurology and psychiatry and director of the Center for Cognitive Aging and Memory Clinical Translational Research, also known as the CAM Center
- Michael Jaffee, M.D., vice chair, department of neurology and director of the Trauma, Concussion and Sports Neuromedicine, or TRACS, program
- Jada Lewis, a professor of neuroscience and coordinator of the Neuroscience Concentration for the Graduate Program in Biomedical Sciences
- Carol Mathews, M.D., a professor of psychiatry and director of the Center for OCD, Anxiety and Related Disorders
- Duane Mitchell, M.D., Ph.D., a professor of neurosurgery, co-director of the Preston A. Wells Jr. Center for Brain Tumor Therapy and director of the UF Brain Tumor Immunotherapy Program
- Gordon Mitchell, Ph.D., a professor of physical therapy and director of the Center for Respiratory Research and Rehabilitation
- Laura Ranum, Ph.D., a professor of molecular genetics and microbiology and director of the Center for NeuroGenetics
New initiatives conceived by the larger MBI executive committee to help support educational and outreach activities are now underway. These activities are designed to further enhance neuroscience education, achieve greater diversity in training opportunities and promote our science both within and outside the university. All of these activities will enrich the McKnight Brain Research Foundation-supported programs. Further, we now have a dedicated science writer, Michelle Jaffee, and a new assistant director of communications, Todd Taylor, to help support these activities and publicize our work. This will include outreach via social media and other outlets.
Notably, the newly formed Outreach and Education Committee, led jointly by Drs. Bizon and Lewis, launched several new programs to serve the UF neuroscience community. These include:
- MBI Research Evenings are events organized thematically that include short presentations by UF neuroscientists, provide an opportunity to highlight research findings and promote collaborations among the UF neuroscience community.
- Trainee Enhancement Opportunities are similar to UF Faculty Enhancement Opportunities in that they will allow research fellows, clinical fellows and graduate students to diversify their skill sets by attending courses, learning new techniques or exploring new aspects of neuroscience not available in their home labs.
- Toffler Leadership Awards fund neuroscience research, education and leadership pursuits by graduate and professional students enrolled in Ph.D., M.D. and M.D./Ph.D. combined programs.
- Our Summer Neuroscience Internship Program, or SNIP, has already trained two dozen undergraduates, including many underrepresented minority students (approximately 60 percent). This program is led by Dr. Lewis and Sara Burke, Ph.D., an assistant professor of neuroscience.
- Our Research Fellowship Program provides pilot funds to trainees and junior scientists, with the goal of stimulating their growth.
- MBI Travel Awards assist UF neuroscientists lacking sufficient resources to present their research at national and international conferences.
- The MBI Neuromedicine Scholars Program, led by Dr. Gordon Mitchell, will bring current and rising stars in the international neuroscientist community to UF. These visits will raise the profile of UF neuroscience and create new opportunities for trainee and community engagement.
Our overall vision for the MBI is to support neuroscience and neuromedicine research across the campus, but to do so in a programmatic way. Our education and outreach efforts are reflective of this vision. Such activities support the entire UF neuroscience community and provide visibility for our individual research programs and neuroscience research centers. As we launch other initiatives, we hope to provide additional infrastructure and resources to support our outstanding thematic science. Numerous neuroscience-related research centers are flourishing and have developed their own unique identity. Established centers are getting more funding, and programmatic grants are being renewed (i.e., Laura Ranum, Ph.D., director of the UF Center for NeuroGenetics, and Maury Swanson, Ph.D., associate director of the UF Center of NeuroGenetics, renewed a P01 grant related to the central nervous system effects of myotonic dystrophy). Newer centers such as the Center for Respiratory Research and Rehabilitation, or CRRR, led by Dr. Gordon Mitchell, are also making great headway. The CRRR provided key support for a large grant from the office of the NIH director to map peripheral and central circuits for airway protection and breathing to Donald Bolser, Ph.D., a professor of physiologic sciences, to study functional mapping of peripheral and central circuits for airway protection and breathing.
We are currently in the early phases of a strategic planning process based on programmatic initiatives. These individual plans will then be synthesized into a larger MBI strategic plan that will provide a road map for the neuroscience community, and hopefully enable us to identify and then fill gaps in expertise, infrastructure or core services. Neuroscience at UF is on a remarkable trajectory and we plan to continue its rise. These are exciting times for our science and discovery in neuroscience, and our team approach is paying off.

UF Health Shands (Shands Teaching Hospital and Clinics Inc.)
CEO: Ed Jimenez, M.B.A.
We concluded another fascinating year for UF Health Shands, with our share of accomplishments, successes and improvements. I want to extend the most sincere gratitude to our hospital-based staff of more than 9,600 employees and 2,200 volunteers. Their unwavering commitment to our patients, visitors and community — and each other — is at the heart of our progress.
Strategic Growth
The most complex and impressive endeavor of 2017, involving many faculty and staff, was opening two new hospitals on Dec. 10 — the UF Health Heart & Vascular Hospital and the UF Health Neuromedicine Hospital. Patients with complex health conditions now receive inpatient and outpatient specialty care from interdisciplinary teams co-located in specially designed spaces unique to their needs. This milestone was the culmination of months of increasingly intense planning and preparations. It took incredible collaboration and cooperation, patience and tireless work. A transition steering team led five subcommittees: Communications, IT, Orientation, Patient Care and Support Services. Hundreds of faculty and staff were involved in the incredibly detailed transition planning process.


Meanwhile, UF Health entered into a formal affiliation with Sacred Heart in Pensacola early last year to provide residency training, pediatric subspecialty care and neonatal and pediatric critical care transport through the UF Health ShandsCair program. Now ShandsCair will lead the ground and air transport of pediatric patients in the Panhandle and offer a service that can fly faster and farther than Sacred Heart’s previous air ambulance. In the event a critically injured child requires a level of care only available at UF Health Shands Children’s Hospital, ShandsCair can fly from Pensacola to Gainesville without stopping to refuel, which could ultimately save the patient’s life. These services join the already existing relationship with Sacred Heart in adult kidney transplantation.

The UF Health ShandsCair program and the Sacred Heart Health System celebrated a new collaboration last fall. Our emergency transport vehicles, pictured here at the Innisfree Jet Center in Pensacola, will help critically ill neonatal and pediatric patients across Northwest Florida quickly access specialized medical care.
Clinical Excellence
Early last year, a patient received what he called a “bionic eye” — a microelectrode array implanted in the retina — here at UF Health Shands Hospital. The electrode assumes the function of damaged retinal cells, sending signals to a special pair of glasses that allows the patient to see shapes and contrasting images. This was our first patient to receive the Argus II Retinal Prosthesis System, and our hospital was one of only 18 implant sites in the U.S.
Last year, families of infants diagnosed with high-risk single ventricle heart defects went home with specially configured iPads and apps that help send important real-time monitoring data to their UF Health care team. Our team at the UF Health Congenital Heart Center, part of UF Health Shands Children’s Hospital, was first in the state to use this technology.
In the fall, three pharmacy technician trainees became the first graduates from the nine-week Pharmacy Technician Training Program — a new collaboration between UF Health Shands Pharmacy Services and the UF College of Pharmacy.
In February, we opened the UF Health Shands Children’s Hospital Neonatal ICU, newly renovated space for our tiniest, most vulnerable patients and their families. It expanded the NICU from 12,632 square feet to 20,844 square feet. The new environment is soothing and family friendly and supports the team’s exceptional clinical care.


Another example of pioneering clinical care last year was when a UF orthopaedic surgeon was one of only two nationwide to perform the first computer-assisted shoulder replacement surgery using a new technology allowing live navigation of the operative site. The technology, ExactechGPS® Total Shoulder Application, provides surgeons with a real-time 3-D computer model of a patient’s shoulder during surgery.
Last spring, we celebrated several hundred UF Health Shands employees for their long-term commitment at our Milestone Service Awards event. Our featured honoree was Rhea Broyles, M.S.N., R.N., for 45 years of service. She started her career as a nurse at Alachua General Hospital and concluded it as a senior quality improvement specialist with the UF Health Sebastian Ferrero Office of Clinical Quality and Patient Safety.
Awards and Recognition
Last year, our UF Health Shands nursing teams received continued national recognition. The Trauma/Lung Transplant Unit nursing team earned their second gold Beacon Award for Excellence from the American Association of Critical-Care Nurses. We now have five active Beacon Awards, and UF Health Shands is tied for first in the Florida to have the most current gold-level Beacon Awards. Our other Beacon-awarded nursing units are the Cardiac ICU (gold), the Pediatric ICU (gold), the Surgical/Trauma ICU (gold) and the Post Anesthesia Care Unit (silver).
In the fall, our UF Health Shands Nursing and Patient Services teams applied for our fourth consecutive Magnet designation. This is the health care industry’s top honor for quality patient care, nursing excellence and innovations in professional nursing practice.
In March, UF Health Shands Hospital earned the highest rating from The Society of Thoracic Surgeons for our patient care and outcomes in congenital heart surgery. The distinguished three-star rating places the hospital among the elite in the U.S. and Canada for congenital heart surgery.
For the third consecutive year, UF Health Shands placed in the U.S. News & World Report annual rankings among the nation’s best in more adult and pediatric medical specialties than any other hospital in Florida. UF Health Shands Hospital and UF Health Shands Children’s Hospital ranked among America’s Best Hospitals and America’s Best Children’s Hospitals, respectively, in six medical specialties each.
We continue to be recognized as a top employer of choice: UF Health placed 21st in Indeed.com’s 2017 Best Places to Work ranking among U.S. hospitals or health systems.
Hospitality and Service
Monthly Hospitality Huddles are now commonplace at UF Health Shands, the College of Medicine and UF Health Physicians. They help us focus on specific hospitality behaviors, outlined by the UF Health Hospitality & Service program, to help us build a supportive and welcoming culture for patients, visitors and staff.
To improve our patients’ experience, UF Health Shands and UF Health Physicians introduced a new user-friendly paperless billing tool in the fall. Patients can view statements online any time, receive email or text notifications when new statements are available or payments are due, and set up their own payment plans.
Late fall, we launched iCARE: A Clean And Restful Environment initiative. Hospital and College of Medicine leaders asked faculty, residents, staff and volunteers to help keep care areas and workplaces clean and tidy, and to be sensitive to noise levels on inpatient units. Staff now use spill stations for immediate clean-ups and some have “adopted” areas such as stairwells to help make a great impression for everyone in our buildings.
Collaboration and Resources
Our UF Health Shands TransLoc Rider app launched in January, providing patients, visitors and staff with a convenient user-friendly tool to track hospital shuttle routes. On computers and mobile devices, users can view the real-time location of our shuttles and see when they will arrive at stops.
We also launched the UF Health Protect personal safety app last year for use by faculty, staff and students. It connects users with digital tools to help keep them safe and help them quickly access emergency resources.
Last spring, the Sixth Annual UF-UF Health Shands Wellness Event was a great success, with increased participation to reach staff and support their well-being. We had an improved overall wellness score of 73 and a 21 percent participation increase, with more than 3,000 employees attending events at 10 onsite locations. Engagement in year-round wellness programs increased: More than 800 employees participated in the 12 Tweaks program, more than 600 completed a workplace-sponsored challenge and around 400 participated in a wellness seminar.
Further progress in engagement was clear: In March, we reached another milestone with 8,345 employees completing the annual UF Health Shands Employee Engagement Survey. That equals 84 percent participation, which is outstanding. Our overall engagement score was 4.26 (out of 5), putting us in the 86th percentile among academic health centers nationwide. This reflects that employees feel valued and trust that leaders appreciate and will use their feedback.
Our employees demonstrated continued altruistic support for local efforts to improve community health. They volunteered, participated in events and raised money. In April, 31 UF Health teams raised $54,000 for the March of Dimes March for Babies. UF Health received the Gold Boot as the area’s No. 1 fundraising team. In September, 724 members of the UF Health family showed their commitment to the American Heart Association’s Alachua County Heart Walk, making us the top fundraising company for the sixth consecutive year. The 39 UF Health teams raised almost $40,000, and together, the community raised more than $224,000 to support the AHA. In October, our UF Health teams supported the American Cancer Society’s Making Strides Against Breast Cancer event. Eighteen UF Health teams raised over $15,000, making UF Health the top local contributor, contributing to the overall total of over $100,000 to support innovative breast cancer research.
Last fall, our UF Health Shands “UNITE” campaign generated more than $228,000 of support from our employees for the United Way of North Central Florida. The funds will help support critical community-based programs that assist families and individuals.
In 2017, our own UF Health Raising Hope at Work campaign raised more than $200,000 thanks to nearly 1,800 UF Health Shands and UF College of Medicine faculty and staff who chose to support projects that directly impact education and patient care. Every Raising Hope at Work dollar generated is invested into our organization.
We experienced another remarkable year of growth, expansion and collaboration. When the going gets tough, our faculty and staff rise to the occasion. This past fall we faced a threatening storm season when Hurricane Irma disrupted regular clinical operations and put our loved ones and homes at risk. The kind of selfless action and commitment we saw from our faculty and staff during that time is just an example of how our people remain positive and engaged in our mission to take care of others. No matter the challenges, everyone across the UF Health family stays focused on what’s needed to provide our patients, visitors and each other with the best possible experience in our organization.
We owe our success to each person in the UF Health family who comes to work every day ready to make a difference. Because of their important work, people who need help and healing can come to UF Health for outstanding medicine and compassionate caring. Each employee contributes to our success as we change lives for the better. I’m filled with admiration and respect for my colleagues across the organization.
Here’s to another great year in 2018 — Go Gators!

UF Health Jacksonville
CEO: Leon L. Haley Jr., M.D., MHSA, C.P.E., FACEP
New CEO for UF Health Jacksonville
Leon L. Haley Jr., MD, MHSA, CPE, FACEP, was named chief executive officer of UF Health Jacksonville following a vote of the organization’s board of directors in September. The appointment came less than a year after Dr. Haley was named dean of the University of Florida College of Medicine – Jacksonville, a position he will continue to hold. Dr. Haley officially assumed his new role on Jan. 1, after former CEO Russ Armistead retired at the end of December.
A new hospital for North Jacksonville
May marked a momentous milestone with the opening of UF Health North’s new 92-bed hospital. This is the first hospital UF Health has designed and built from the ground up in Jacksonville. It is also the only hospital in North Jacksonville.
Suites at UF Health North are designed to make patients as comfortable as possible while they heal. Each room has large windows to fill it with natural light and has a view of the outdoor courtyard, pond or rooftop garden. Suites are equipped with interactive technology using a tablet and speaker synced with the 55-inch TV, allowing patients to watch television and movies, order meals, contact nursing staff, view upcoming tests and more. Many waiting lounges are connected to balconies, so visitors can get fresh air. Two floors connect to the neighboring medical office building for easy transfer and patient navigation.


Like the medical office building, the hospital’s contemporary design draws on the wetlands in the region. Pieces from local artists decorate the interior, including murals near nurses’ stations and photography used as cabinet doors to conceal medical supplies. The courtyard features seating surrounded by greenery. The chapel is nearby, with plenty of windows for sunlight. Four conference rooms are available for public use to hold meetings and can be opened into a single space for larger events.
North hospital by the numbers:
- Dedicated obstetric operating rooms: 2
- Women’s services private rooms: 8
- Labor and delivery suites: 12
- Intensive care unit rooms: 24
- Medical/surgical rooms: 48
- Square feet: 168,000
North’s new baby
UF Health North opened its 12 labor and delivery suites in August. They also serve as recovery and postpartum rooms, so mothers can remain comfortable during their stay. Three of these suites feature hydrotherapy tubs. The nursery is located directly next to the nurses’ station, but the suites are spacious enough for babies to remain in their mothers’ rooms while still accommodating family and friends. Two dedicated obstetric operating rooms are also located on the unit for mothers in need of a planned or unplanned cesarean section.

We delivered our 100th baby in December.
Employee engagement survey results
By measuring and improving employee engagement, we work together to create a healthy and healing environment that produces excellent care and service. Nearly 3,200 staff completed the confidential online survey in August. With a 72 percent response rate, we ranked in the 65th percentile for engagement compared with the national health care average.
Our most significant improvements compared with the 2016 survey included the ability of employees to disconnect from work communications during free time and work-life balance (the ability to separate from work during personal time). Improvements in trust within employees’ work units and knowing their work makes a difference also made the list. Salaries and career development opportunities were identified as strengths by employees.
Hurricane Irma response
Last year was a particularly active hurricane season, with several storms causing widespread devastation in multiple states as well as small islands south of Florida. We were fortunate to avoid a direct hit from Hurricane Irma, however, heavy rains and high winds caused significant damage in the community.
Incident command centers at UF Health Jacksonville and UF Health North worked together to ensure clinical operations continued without interruption and communicated with managers and directors around the clock. Water leaks, power outages, staffing levels, disaster linens and sleeping accommodations for overnight staff were among the concerns addressed. More than 30 UF Health physicians, nurses and respiratory therapists volunteered to staff one of the city’s busiest special-needs shelters.
While other hospitals in the area were unable to take patients — many needing emergency treatment — UF Health Jacksonville and UF Health North remained open to care for every patient who came through our doors.
UF Health Rehabilitation – Emerson expansion
UF Health Rehabilitation – Emerson nearly tripled in size last December, when it moved into a new 10,000-square-foot facility. More space enables the Emerson location to offer specialty rehabilitation services such as neurology, sports, oncology, women’s health and speech therapy, in addition to the musculoskeletal orthopaedic care it was already providing.
There are two therapy gyms — one designed for orthopaedic and sports rehab patients and another for patients with neurologic conditions — equipped with some of the latest rehabilitation technology available today. Both gyms have a ceiling-mounted body-weight support system that includes a harness to prevent patients from falling, while therapists work with them to improve their balance, gait, motor function and lower body strength. The system can help increase early mobility and enables patients to get a sense of what it feels like to stand and walk on their own, instead of relying on another person for support. Both areas are connected by private therapy rooms. A speech therapy room has special acoustics and equipment to capture sounds and give auditory biofeedback to accelerate therapy goals.

The orthopaedic and sports rehab gym includes a designated area with turf and protective sports netting for injured athletes who are in the final phases of their rehabilitation program to practice the mechanics of their sports, such as football, baseball and golf. Therapists are building on the existing sports therapy services by adding ACL injury prevention and post-concussion rehabilitation.

The second gym was designed so that more services can be offered to patients with neurologic conditions. Neurology specialists provide customized balance, occupational, physical and speech therapy for patients recovering from traumatic head and spine injuries, stroke and other neurological conditions. Advanced equipment is used, such as an electrical stimulation bike, a computerized balance machine and the ceiling-hung suspension system.
Four stars for quality care
National health care research leader Professional Research Consultants Inc. recognized UF Health Jacksonville with an Excellence in Healthcare Award at its Excellence in Healthcare Conference in June.
UF Health Jacksonville’s Emergency Department achieved a four-star rating for overall quality of care in all department areas, including trauma, pediatrics and the UF Health North Emergency Department. PRC singled out several UF Health Jacksonville departments as individual best performers, including Inpatient Psychiatry and the Cardiovascular Intensive Care Unit. PRC also recognized the UF Health North Emergency Department and Outpatient Surgery as best performers.
The Excellence in Healthcare Awards recognize organizations and individuals who achieve excellence throughout the year by improving the patient experience as well as employee and physician engagement.
UF Health North awarded certificate of distinction by The Joint Commission
The Joint Commission awarded UF Health North a Certificate of Distinction for advanced certification as an Acute Stroke-Ready facility. The commission based its decision on a review of UF Health North’s compliance with national standards, clinical guidelines and outcomes of care. Acute Stroke-Ready certification recognizes hospitals that meet standards to achieve better outcomes as part of a stroke system of care.
UF Health Jacksonville was recertified as a Primary Stroke Center by The Joint Commission last year.
MICU earns a Silver Beacon Award
UF Health Jacksonville’s Medical Intensive Care Unit was recognized by the American Association of Critical-Care Nurses in May. The association awarded the unit a 2017 Silver Beacon Award for Excellence — the first unit at UF Health Jacksonville to receive this award. The honor is given to the country’s top nursing units that improve patient outcomes and align their practices with the AACN’s Six Healthy Work Environment standards.
High rankings from U.S. News & World Report
UF Health Jacksonville was ranked among the best hospitals for 2017-18 in a U.S. News & World Report comparison of hospitals across the nation. Highlighting the organization’s achievements is its ear, nose and throat program, which is ranked 37th best in the United States. We were also recognized as a “Best Hospital” in northern Florida and received high-performing scores in three other specialties: nephrology, heart failure and chronic obstructive pulmonary disease.
Rising up the ranks for patient safety efforts
UF Health Jacksonville’s ranking among academic health centers in the United States jumped significantly in 2017, rising 33 spots in the latest Vizient rankings. UF Health Jacksonville is now ranked 44th in the country, with major improvements in five of the six categories measured: mortality, effectiveness, safety, efficiency and equity.
UF Health Jacksonville’s improvements over the past several years have been dramatic in many areas of patient safety. Since 2014, the hospital has seen a 52 percent decrease in its mortality index, a 66 percent decrease in central line infections, a 74 percent decrease in urinary tract infections, a 57 percent decrease in pressure ulcers, a 78 percent decrease in respiratory failure, a 70 percent decrease in surgical infections and an 88 percent decrease in bleeding events.
Finances
Despite the financial impact caused by Hurricane Irma and state funding challenges, UF Health Jacksonville is slightly ahead of our budget target for the first half of fiscal year 2018 (July through December 2017).
Looking forward
We expect 2018 to be a great year as we continue our growth throughout North Jacksonville and surrounding areas. We look forward to providing high-quality, compassionate care to our patients and their loved ones. Working together, we will fulfill our vision to be the region’s most valued health care asset.
Concluding remarks
The breadth and depth of the achievements of faculty and staff at our academic health center, as summarized in this “Year in Review,” is always humbling and inspiring. It doesn’t get old! Moreover, the trajectory of our success has not reached a plateau. Indeed, building on the amazing progress highlighted across all of our colleges, research institutes and hospitals, I am confident that the best is yet to come. I wish you all the very best for 2018 and look forward to working with you to achieve our collective goals.
Power of Together,
David S. Guzick, M.D., Ph.D. Senior Vice President for Health Affairs, UF President, UF Health
About the author
