Enhancing Quality While Accommodating Growth
At UF Health, quality is Job 1. Our goal is to deliver exceptional service, value and quality to every patient at every encounter.
Over the past several years, as our reputation for quality care, hospitality and service has grown, more patients are choosing UF Health for medical care. New clinical faculty members were hired to accommodate this growth, along with nurses and other staff. But we can only grow so much, at least regarding inpatient services, within a fixed chassis. The new UF Health Neuromedicine Hospital and UF Health Heart & Vascular Hospital reflect our recognition that new facilities are needed to accommodate continued growth.
But what do we do in the meantime? How can we enhance quality when we’re already full to the brim and more patients are at the door seeking our services? Our success has created a challenge: Satisfaction will not be high if our patients are waiting several hours in the Emergency Room for an inpatient bed; and the gridlock of a full hospital compromises our ability to complete lab and imaging studies efficiently, leading to longer hospital stays. Longer hospital stays, in turn, mean there are fewer beds available for hospital-to-hospital transfers and for patients in the ER who need to be admitted. To address this challenge, we need to reduce length of stay, or LOS, to accommodate growth, while increasing quality and patient satisfaction at the same time.
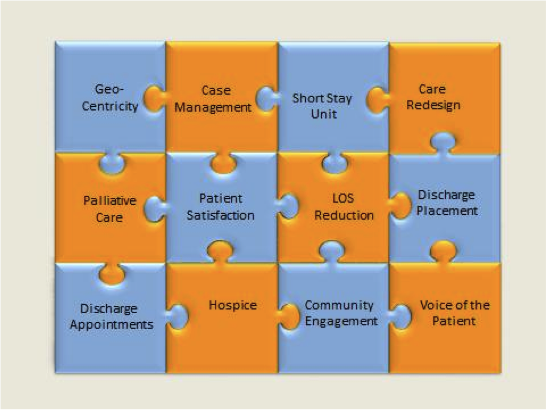
Many aspects of our patient care enterprise impact LOS and patient satisfaction. Chief Quality Officer Randy Harmatz has pictured this as a jigsaw puzzle, shown below. LOS and patient satisfaction are at the center of the jigsaw puzzle, but there are many interlocking and interrelated factors impacting these two central factors. In short, we can’t improve patient satisfaction and reduce LOS unless these other interrelated factors are addressed successfully.
Over the past several months, the senior leadership of UF Health — Dean Mike Good, CEO Ed Jimenez, myself and others — have been working diligently on these issues. In December, we visited Duke University Health System, which had just undergone an enterprise-wide restructuring of its approach to patient care processes and other factors with the help of an outside consultant. Over the ensuing months, we explored several individual aspects of patient care represented by pieces of the jigsaw puzzle and agreed on an interdisciplinary approach. On Feb. 9, 2016 we had a three-hour meeting with faculty and hospital leadership responsible for those areas, and on March 12th, we had a full-day retreat to consider how these considerations impact the transition to the new hospitals.
Taking all of the insights gained by these visits, conversations and meetings, on March 18th we convened the faculty and staff who collectively will lead a process in which the pieces of the jigsaw puzzle will be brought together to improve quality and enhance patient satisfaction while accommodating continued growth. A working group has been assigned to each piece of the jigsaw puzzle. These working groups will be co-chaired by a faculty member and hospital administrator, and will be facilitated by a project manager. A steering committee will coordinate and distill the work of the teams. A listing of these working groups and their chairs and project managers can be found here.
A brief summary of the rationale for the working groups is as follows:
- Medicine Geocentricity and short-stay unit: Because there is such pressure to find an available bed for patients waiting to be admitted from the ER, patients are often located on floors other than the “home” for their clinical service. This group will develop processes to ensure that most patients are admitted to their correct “home” location. The seventh floor of UF Health Shands Hospital (hospitalist service) is piloting this program. In addition, last week we began the process of co-locating patients who are projected to require a short stay (i.e., less than two days).
- Case management and discharge placement: Case managers have a variety of professional backgrounds, including nursing and social work. Their common goal is to ensure that all of the family, social and other resources needed by our patients are in place for them to facilitate the transition from discharge to home or wherever their next location might be (e.g., rehab or nursing home). The emphasis here is to create highly reliable systems to ensure that case management planning begins at (or even before) admission and continues throughout the hospital stay with clear and efficient communication among members of the health care team, and that timely discharge of patients with adequate support resources occurs.
- Discharge appointments: Often patients who are admitted to the hospital have not seen a doctor previously. It is important that they are seen soon after discharge by a physician who will provide appropriate follow-up and ongoing care. The goal is for patients to have a follow-up appointment in the Epic system with a specific physician at a specific time and date. This will be piloted on several of the medicine services first.
- Hospice and palliative care: We have not been at the forefront in these services for our patients. Now, under the leadership of Sharon Gavin, M.D., and with the return of Sheri Kittelson, M.D., from her palliative care fellowship in July, we will have the capacity and expertise to create various options for our patients and their families in this important domain.
- Care redesign: To optimize our quality of care, we will seek to reduce variability in a variety of care processes, based on national standards and evidence in the literature. Initially, the focus will be on care processes such as sepsis recognition and early treatment, blood product utilization, laboratory and imaging utilization, ER workflow, and critical care medicine.
- Community engagement: The goal here is to expand successful community partnerships so as to improve care and coordination across the continuum. This may include a variety of programs such as Take Charge, CareOne, UF Health Family Medicine – East Side, HealthStreet and the Archer Clinic, and our community needs assessment will help inform future directions.
- Patient centeredness: There will be two subgroups in the domain, one focused on the assessment/enhancement of patient centeredness in the ambulatory faculty practices, and one focused on similar aspects of the inpatient experience. In this effort, we will engage patients and family members in all levels of care redesign (e.g., wayfinding, technology, etc.).
As we look forward to moving some of our patients into new hospital towers in December 2017, we need to ensure the highest quality of care for the patients we take care of between now and then, and to ensure a smooth transition. If you have any suggestions regarding the topic areas described above, please contact one of the co-chairs of the pertinent work-group. We look forward to hearing from you.
The Power of Together,
David S. Guzick, M.D., Ph.D. Senior Vice President for Health Affairs, UF President, UF Health
About the author
