Laparoscopic and Robotic Nephroureterectomy
For patients diagnosed with transitional cell carcinoma of the kidney or ureter (aka urothelial cell carcinoma), laparoscopic and robotic nephroureterectomy provides patients with a safe and minimally invasive technique for complete removal of the affected kidney, ureter, tumor and regional lymph nodes.
This minimally invasive approach has the advantage of improved cosmesis, reduced pain, blood loss, and hospital stay, as compared to conventional open surgery with similar cure rates.
The Surgery
The Operation
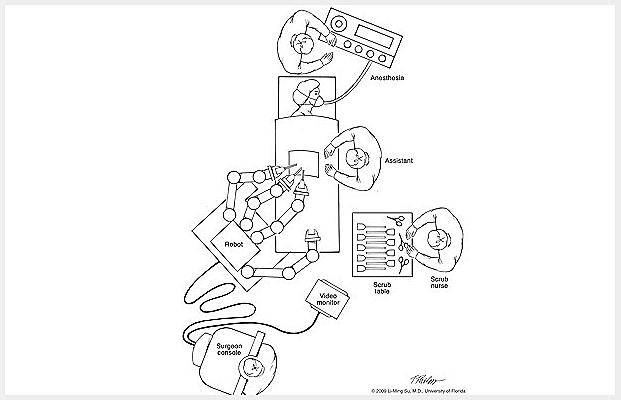
Laparoscopic and robotic nephroureterectomy requires that patients undergo a general anesthesia. While operative time varies from one individual to another, the average operating time is approximately 3-4 hours.
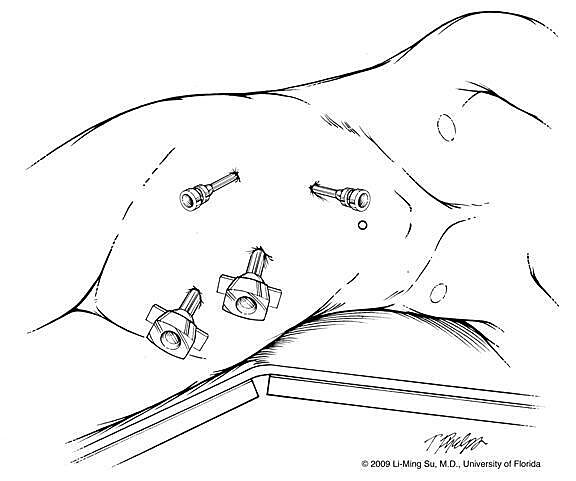
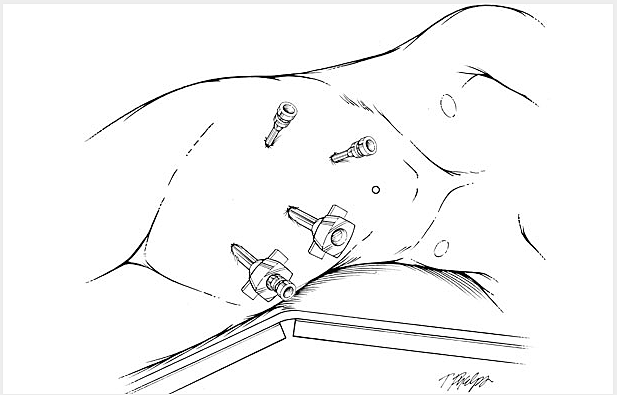
During this procedure approximately 4 small keyhole (< 1cm) incisions are made in the abdomen (Figure 1), which allow the surgeon to insert a telescope (called laparoscope) and miniaturized surgical instruments into the abdomen through portals call trocars.
The laparoscocpe allows for 10X magnification of the operative field, allowing the surgeon to accomplish the surgical procedure with improved visualization and without placing his hands into the abdominal cavity. The abdomen is filled with carbon dioxide gas to create a larger working space for the surgeon to accomplish the operation. This gas is later evacuated from the abdomen at the conclusion of the operation.
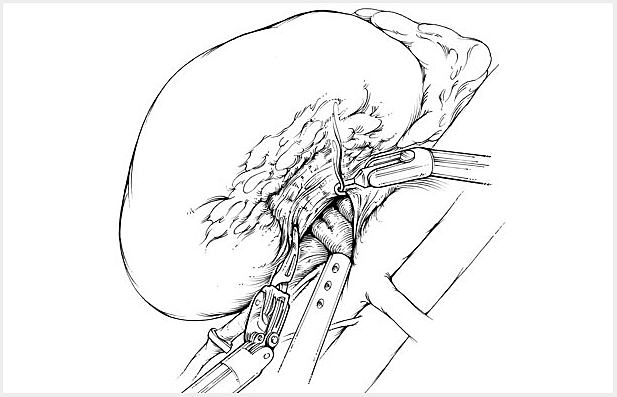
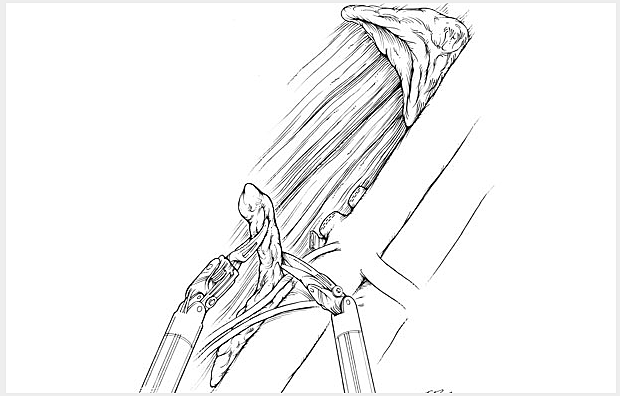
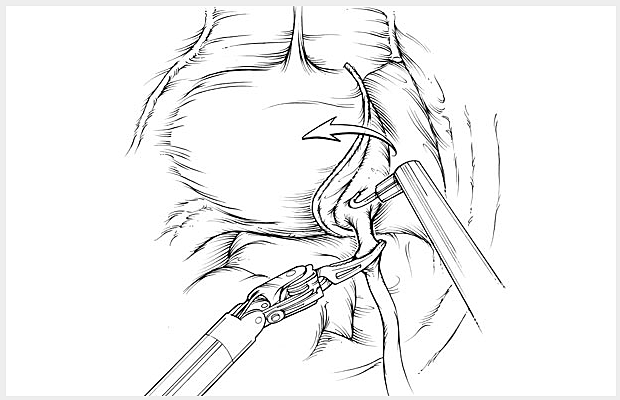
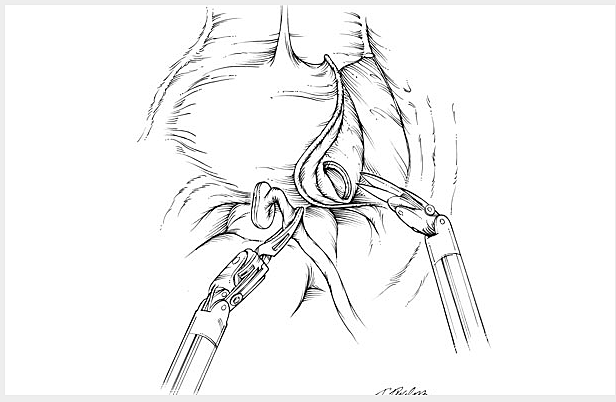
The affected kidney and ureter is then dissected and exposed from surrounding organs such as the liver, spleen and intestines. The blood supply to the kidney is clipped and divided, allowing for safe and efficient removal of the kidney with minimal blood loss. The tumor within the kidney or ureter and surrounding fat and visible surrounding lymph nodes are removed. The adjacent adrenal gland may also at times be removed if the tumor is large or in close proximity to it.
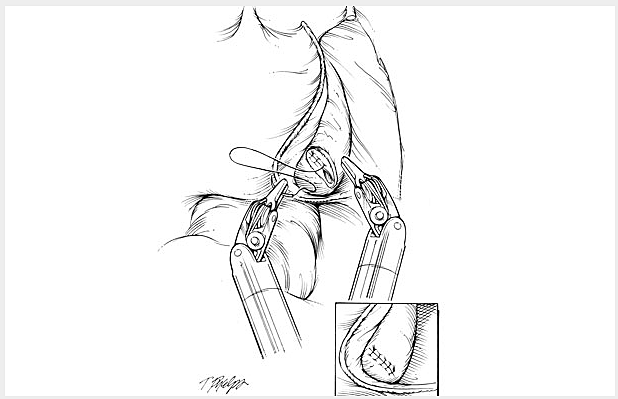
Once the tumor, kidney and ureter are excised, they are immediately placed within a plastic sack and the specimens are removed from the abdomen intact by extraction through one of the pre-existing abdominal incisions. Finally, the skin incisions are closed using plastic surgery techniques to minimize scarring.
Slide Show
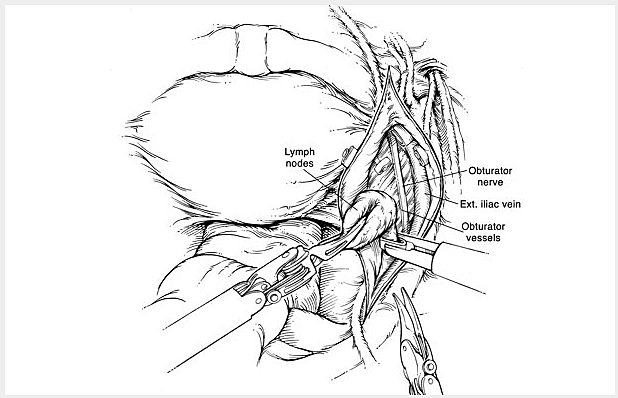
The following is a slide show of a series of schematic drawings to help patients better understand the steps involved with robotic nephroureterectomy.

Potential Risks and Complications
As with any major surgery, complications, although rare, may occur with laparoscopic and robotic nephroureterectomy. Potential risks and complications with this operation include but are not limited to the following:
- Bleeding: Blood loss during this procedure is typically less than 100 cc with the rare need for a blood transfusion (<2% of patients). If you are interested in autologous blood transfusion (donating your own blood) prior to your surgery, you must make your surgeon aware. This can be arranged locally in Gainesville, FL at the Civitan Regional Blood center or at your local Red Cross.
- Infection: Although patients are given broad spectrum intravenous antibiotics immediately prior to surgery, infections of the urinary tract and skin incisions may still occur but are rare. If you develop any signs or symptoms of infection after the surgery (fever, drainage from or redness around your incisions, urinary frequency/discomfort, pain) please contact us at once.
- Adjacent Tissue / Organ Injury: Although uncommon, adjacent organs and tissues may be injured as a result of your surgery. This includes the colon, bowel, vascular structures, nerves, muscles, spleen, liver, pancreas and gallbladder. If injury to your lung cavity occurs, a small chest tube may be required to evacuate air, blood, and fluid from around your lung, thus allowing your lung to expand and work properly. On rare occasions, further surgery may be required to address unexpected injuries to adjacent organs.
- Incisional Hernia: Because of the small laparoscopic incisions, hernias at these sites occur rarely. In addition, larger incisions are closed carefully prior to the completion of your surgery to minimize the risk of hernias.
- Conversion to Open Surgery: In the rare event of complications or due to difficulty in dissecting by means of laparoscopy, conversion to open surgery is sometimes required. This could result in a larger standard open incision and possibly a longer recuperation period.
What to Expect After Surgery
After a period of recovery in the Recovery Room, you will be transported to your hospital room once you are aware and your vital signs stable.
- Postoperative Pain: Although most patients in the first few days after surgery experience mild pain at their incision sites, this is generally well controlled by use of intravenous pain medication, patient-controlled anesthesia pump, or oral pain medication provided by your nurse. You may experience some minor transient shoulder pain (1-2 days) related to the carbon dioxide gas used to inflate your abdomen during the laparoscopic or robotic surgery.
- Nausea: Nausea can occur following any surgery especially those procedures that require general anesthesia. This is usually transient and controlled by medication which can be administered on an as needed basis by your nurse.
- Urinary Catheter: A urinary catheter (also called foley catheter) is placed to drain your bladder at the time of surgery while you are asleep. This is in efforts to monitor your urine output following surgery. It is not uncommon to have blood-tinged urine for a few days after your surgery while your catheter is in place. The catheter generally remains in place for approximately 7-10 days to be removed later in a followup visit in the clinic.
- Diet: Your diet will be advanced slowly following surgery from liquids to solids as tolerated. It is often the case that your appetite will be poor for up to a week following surgery. In addition, your intestinal function is often sluggish due to the effects of surgery and general anesthesia. It is for these two reasons that we recommend taking only small amounts of liquids by mouth at any one time until you begin to pass flatus and your appetite returns. In the meantime, your intravenous catheter will provide the necessary hydration to your body as you oral intake improves.
- Fatigue: Fatigue is quite common following surgery and should subside in a few weeks following surgery.
- Incentive Spirometry: You will be expected to do some very simple breathing exercises to help prevent respiratory infections through using an incentive spirometry device (these exercises will be explained to you by the nursing staff during your hospital stay). Coughing and deep breathing is an important part of your recuperation and helps prevent pneumonia and other pulmonary complications.
- Ambulation: On the evening of surgery it is very important to get out of bed and begin walking with the supervision of your nurse or family member to help prevent blood clots from forming in your legs. You can also expect to have SCD’s (sequential compression devices) wrapped around your lower legs and calf area to prevent blood clots called deep vein thrombosis from forming in your legs. In the days that follow surgery, patients are advised to walk at least 6 separate times a day in the hallways. This serves to further reduce the change of deep vein thrombosis and speed the return of bowel function.
- Constipation/Gas Cramps: You may experience sluggish bowels for several days following surgery as a result of the anesthesia. Suppositories and stool softeners are usually given to help with this problem. Taking a teaspoon of mineral oil daily at home will also help to prevent constipation. Narcotic pain medication can also cause constipation and therefore patients are encouraged to discontinue any narcotic pain medication as soon after surgery as tolerated.
- Hospital Stay: The length of hospital stay following laparoscopic radical nephrectomy is generally 1-2 days.
What to Expect After Discharge from the Hospital
- Pain Control: For the majority of patients, one to two days of oral narcotic pain medication may be necessary after which Extra Strength Tylenol is usually sufficient to manage their pain. Again, narcotics should be minimized to avoid constipation and over sedation.
- Showering: Patients can shower immediately upon discharge from the hospital allowing their incisions to get wet. Once out of the shower, pad your incision sites dry and avoid any heavy creams or lotions. Tub baths or hot tubs in the first 2 weeks are discouraged as this will allow for prolonged soaking of your incisions and increase the risk of infection. You may shower after returning home from the hospital. Your wound sites can get wet, but must be patted dry immediately after showering. The sutures underneath the skin will dissolve in 4-6 weeks.
- Activity: Walking 6 times a day for the first two weeks after surgery on a level surface is strongly encouraged as prolong sitting or lying can increase your risk of pneumonia and deep vein thrombosis. It is permissible to climb stairs. No heavy lifting or exertion for up to 4 weeks following surgery. Patients may begin driving once they are off of narcotic pain medication and have full range of motion at their waist. Most patients can return to full activity including work on an average 3-4 weeks after surgery.
- Diet: Patients may resume a regular diet once they begin to pass flatus and their appetite improves.
- Follow-up Appointment: Patients should make a follow-up appointment with their surgeon by contacting UF Health Urology - Medical Plaza at (352) 265-8240. The precise timing of this appointment will be determined by your surgeon but is generally within 7-10 days following surgery at which point the urinary catheter will be removed.
- Pathology Results: The pathology results from your surgery are usually available in one week following surgery. Your results will be discussed with you either by phone or directly in the office during a follow-up clinic appointment.
Frequently Asked Questions (FAQs)
What is the advantage of laparoscopic and robotic nephroureterectomy as compared to open surgery?
Laparoscopic and robotic nephroureterectomy has translated into a significant benefits to patients including reduced blood loss and transfusions, reduced pain, shorter hospital stays, improved cosmesis, and a faster recovery as compared to open surgery. While open surgery may require 1-2 large abdominal or flank incisions, minimally invasive approaches involve 4 keyhole incisions in the abdomen.
Are there potential disadvantages?
Most patients with transitional cell carcinomas of the kidney and ureter who are candidates for open surgery are also excellent candidates for a laparoscopic or robotic approach. These minimally invasive approaches have become the standard of care for most kidney tumors. In general there are no particular disadvantages, however, some situations may dictate the need for open surgery (see below).
What patients are not good candidates for laparoscopic or robotic nephroureterectomy?
Patients with very large tumors or tumors invading surrounding structures e.g. vena cava, liver, bowel may be best served by an open approach due to the extent and need for adjacent organ resection. Patients with medical conditions such as severe lung and heart disease may not be able to tolerate a laparoscopic approach due to the need to undergo a general anesthetic.
What is the difference between a laparoscopic and robotic approach?
Both are laparoscopic approaches and the choice of approach is a matter of surgeon preference. Operative times, blood loss, and hospital stays are similar between a pure laparoscopic and robotic technique. These procedures are performed by inflating the abdomen with carbon dioxide gas and placing a laparoscopic lens affixed to a high definition camera into the abdomen to view the internal organs. Conventional laparoscopic surgery involves hand held instruments, while robotic surgery involves the use of a sophisticated robotic device (called the da Vinci Surgical Robotic System) with wristed instrumentation to allow the surgeon to dissect within the abdomen while controlling these instruments externally from a surgeon console.
What happens if complications arise and conversion to open surgery is required?
Although extremely rare, conversion to open surgery may be required if difficulty with dissection is encountered during the laparoscopic approach. Our surgeons are trained in open surgical approaches as well as laparoscopy and therefore are well equipped to complete the surgery in an open fashion if needed.
What is the overall success rate of laparoscopic and robotic nephroureterectomy?
Success rate in complete removal of the tumor is identical to open surgical approaches. Prognosis of cancer-free survival is based upon the grade, stage and particular type of your cancer and will be discussed with you by your surgeon upon review of your pathology report. These results will be available approximately one week after surgery.
Will I need further treatment such as radiation or chemotherapy following surgery?
For patients with low grade, contained tumors, prognosis remains excellent as most are cured with surgery alone. Rarely, patients are found to have large, invasive cancers that may require adjuvant treatment with chemotherapy.
These would be administrated under advisement of a medical oncologist.
